Crohn's Disease in Women: Symptoms, Hormonal Impacts & Daily Management
Let's talk about Crohn's disease in women. It's a topic that doesn't always get the spotlight it deserves in general discussions about inflammatory bowel disease (IBD). If you're a woman living with Crohn's, you might have noticed your experience doesn't always match the textbook descriptions. You're not imagining things. The way Crohn's disease manifests, progresses, and interacts with your life can be profoundly different because you're a woman. Hormones, reproductive health, societal roles – they all weave into the fabric of your daily management in a way that's uniquely challenging.
I remember speaking with a gastroenterologist who mentioned, offhand, that women often report a different set of struggles. It wasn't just about the location of inflammation. It was about everything around the disease. That conversation stuck with me. So, let's dive in and unpack what Crohn's disease in women really entails, beyond the basic medical facts.
How Symptoms of Crohn's Disease Show Up Differently in Women
You'll see the classic symptoms listed everywhere: abdominal pain, persistent diarrhea, weight loss, fatigue. And yes, women with Crohn's disease absolutely get those. But there's a layer underneath that. The presentation can be subtler, or sometimes, confusingly intertwined with other female-specific health issues.
For instance, pelvic pain. It's a big one. When inflammation is in the lower end of the digestive tract (ileum or colon), the pain can radiate or be mistaken for gynecological pain. I've heard stories of women spending years being treated for suspected endometriosis or ovarian cysts before someone thought to look at their intestines. That's a frustrating and exhausting diagnostic odyssey no one should have to endure.
Then there's the fatigue. Oh, the fatigue. It's a universal symptom, but when you layer it on top of the physical demands many women face – whether from work, caregiving, or both – it can be utterly debilitating. It's not just "feeling tired." It's a bone-deep exhaustion that makes even simple tasks feel like climbing a mountain. And society isn't always kind to women who need to rest.
Iron-deficiency anemia is another silent companion for many women with Crohn's. Between blood loss from intestinal inflammation and the monthly menstrual cycle, iron stores can take a serious hit. The result? Paleness, dizziness, shortness of breath, and that fatigue feeling even worse. It's a vicious cycle that needs proactive management.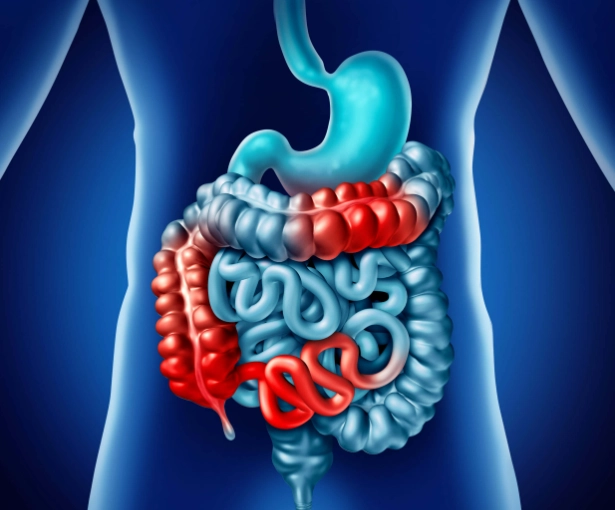
The Menstrual Cycle Connection: It's Not in Your Head
If you've ever felt your Crohn's symptoms ramp up right before your period, you're not making it up. There's a real, biological link. Fluctuating levels of estrogen and progesterone throughout the cycle can directly influence gut motility, pain perception, and even immune system activity.
Many women report a premenstrual flare. Cramps get worse, diarrhea increases, and overall discomfort peaks. It's like your body is dealing with two separate inflammatory events at once. Tracking your symptoms alongside your cycle can be a game-changer. It helps you predict tougher days and plan accordingly – maybe you clear your social calendar for that weekend, or ensure your work schedule is light.
What about hormonal contraceptives? The research is mixed. Some older studies suggested a potential increased risk of flare with certain oral contraceptives, but newer data isn't as clear-cut. The Crohn's & Colitis Foundation states that for most women with IBD, modern low-dose birth control pills are considered safe and effective. However, this is a crucial conversation to have with both your gastroenterologist and your gynecologist. They need to work together. If you have active disease or a history of blood clots, the decision needs extra care.
Fertility, Pregnancy, and Crohn's Disease: What You Need to Know
This is often the biggest source of anxiety for young women diagnosed with Crohn's disease. Let's clear the air on a major myth first: Having Crohn's disease does not mean you cannot have children. In fact, when the disease is in remission, fertility rates for women with Crohn's are comparable to those without the disease.
The real issue is active disease. Inflammation, poor nutrition, and the stress of an active flare can reduce fertility. So, the single most important thing you can do if you're planning a pregnancy is to work towards and achieve remission before you start trying. This isn't just a nice-to-have; it's critical for your health and the baby's.
Now, onto medications. This fear stops many women in their tracks. They worry their meds will harm a baby and stop taking them, which often leads to a devastating flare during pregnancy. That scenario is far riskier than most maintenance medications.
Let's look at some common drug categories:
| Medication Type | Common Examples | General Safety Profile in Pregnancy* | Key Consideration for Women |
|---|---|---|---|
| Aminosalicylates | Mesalamine, Sulfasalazine | Generally considered safe. Sulfasalazine requires extra folic acid. | Often continued throughout pregnancy to maintain remission. |
| Corticosteroids | Prednisone, Budesonide | Used for treating flares. Associated with a small risk of cleft palate if used in first trimester; benefits often outweigh risks in active disease. | Goal is to avoid flares to minimize need for steroids. |
| Immunomodulators | Azathioprine, 6-MP | Extensive data suggests they are generally safe. Continuing is usually recommended to prevent flare. | Stopping these meds carries a high risk of relapse. |
| Biologics | Anti-TNFs (Infliximab, Adalimumab), Vedolizumab, Ustekinumab | Most cross the placenta, especially in 3rd trimester. However, keeping mother healthy is paramount. Often continued, with timing of last dose before delivery planned. | Baby may have detectable drug levels at birth, affecting live vaccine schedules. Crucial to plan with a high-risk OB and GI. |
*This table is a simplified overview. Medication decisions must be made individually with your healthcare team.
The consensus from major organizations like the American College of Obstetricians and Gynecologists (ACOG) and the Crohn's & Colitis Foundation is clear: A healthy mother is the best predictor of a healthy pregnancy. Staying on effective maintenance therapy is almost always the recommended path. You need a high-risk obstetrician who is familiar with IBD and a gastroenterologist who communicates with them. Don't settle for less.
Pregnancy itself is fascinating. For many women whose Crohn's is in remission at conception, they have a great chance of staying in remission throughout the pregnancy. Some even feel better than ever! However, for those with active disease at conception, the course can be more complicated. Postpartum is another key time. The hormone crash and sleep deprivation can trigger a flare, so having a support plan in place is essential.
Daily Life and Long-Term Management for Women
Managing Crohn's disease in women isn't just about pills and procedures. It's about navigating the world, relationships, and your own body image. Let's get practical.
Diet and Nutrition: Beyond the Basics
There's no one "Crohn's diet." What triggers one person may be fine for another. The common advice is to keep a detailed food diary. But for women, pay extra attention to how your cycle affects your tolerance. You might handle salads just fine most of the month, but find they're impossible during your period.
Calcium and Vitamin D are non-negotiable. Women are at higher risk for osteoporosis anyway, and the combination of chronic inflammation and possible long-term steroid use amplifies that risk. If you're lactose intolerant (common with Crohn's), you need to find other sources – fortified plant milks, canned fish with bones, leafy greens (if you tolerate them), or talk to your doctor about supplements.
Body image and weight fluctuations can be brutal. The prednisone bloat, the sudden weight loss from a flare, the scars from surgery… it takes a toll. Social media doesn't help. Finding a community of other women with IBD, whether online or in person, can be incredibly validating. They get it in a way others simply can't.
Mental and Emotional Health: The Invisible Burden
Anxiety and depression are more common in people with IBD, and women are statistically more likely to experience them. It's not weakness; it's a physiological and psychological response to a chronic, unpredictable illness. The constant planning around bathroom access ("Where's the nearest toilet?"), the fear of public accidents, the fatigue that makes you cancel plans – it's isolating.
Seeking therapy, particularly from someone experienced in chronic illness, is a sign of strength, not failure. Cognitive Behavioral Therapy (CBT) has good evidence for helping manage the anxiety associated with IBD. Mindfulness and meditation can also help with pain perception and stress. And sometimes, medication for anxiety or depression is the right tool for the job. Your brain is part of your body, and it deserves care too.
Relationships can be strained. Partners may struggle to understand the invisible symptoms. Friends may think you're flaky. It's exhausting to constantly educate people. Having a few simple, honest phrases ready can help: "My chronic illness is acting up today, so I need to rest" or "I'd love to see you, but I need a raincheck." True friends will understand.
Quick-Reference: Management Checklist for Women with Crohn's
- Medical Team: Ensure you have a supportive gastroenterologist. Consider adding a high-risk OB/GYN if planning pregnancy, a registered dietitian, and a therapist.
- Tracking: Use an app or journal to track symptoms, menstrual cycle, food, and stress. Look for patterns.
- Bone Health: Discuss a DEXA scan with your doctor to check bone density. Prioritize calcium and Vitamin D.
- Vaccinations: Stay up-to-date, especially with flu and pneumonia shots. Discuss live vaccines (like MMR) if on biologics.
- Support System: Build your team – understanding family/friends, online IBD communities, local support groups.
- Self-Advocacy: Practice speaking up for your needs at work (consider ADA accommodations) and in medical settings.
Addressing Common Questions and Concerns
Let's tackle some of the specific questions that pop up again and again when women search for information about Crohn's disease.
Does having Crohn's disease increase my risk for gynecological cancers? The research here is ongoing and complex. There does appear to be a slightly increased risk of cervical dysplasia (pre-cancerous cells) in women with IBD, possibly linked to immune system function. This makes regular Pap smears absolutely essential. The risk for ovarian or uterine cancer isn't as clearly elevated, but maintaining routine gynecological care is non-negotiable. The Centers for Disease Control and Prevention (CDC) guidelines for cancer screening are a good baseline, but your doctors may recommend more frequent checks.
Can I have a vaginal delivery if I've had Crohn's-related rectal surgery or perianal disease? This is a major decision. If you have active perianal disease (fistulas, abscesses), a C-section is usually recommended to avoid trauma to the area and the risk of creating new fistulas or injuring the anal sphincter. For women with a history of ileal pouch-anal anastomosis (IPAA or J-pouch), the data is mixed, and the decision depends on the health of the pouch and pelvic floor. This requires a detailed discussion with your surgeon, GI, and OB.
Is menopause different for women with Crohn's? It's an understudied area, but an important one. The drop in estrogen during menopause can affect bone density loss, which is already a concern. Some women report a change in their Crohn's symptoms post-menopause – for better or worse. Hormone Replacement Therapy (HRT) is a personal decision that comes with its own risks and benefits; having Crohn's adds another factor to weigh with your doctors.
How do I handle intimacy and sexual health? Pain during intercourse (dyspareunia) can occur, especially if there is pelvic inflammation or scarring from surgery. Fatigue and poor body image are also major libido-killers. Open communication with your partner is key. Sometimes, simply changing positions can help. Don't suffer in silence; this is a valid medical concern to discuss with your GI or gynecologist.
Putting It All Together: Your Path Forward
Living with Crohn's disease as a woman requires a multifaceted approach. You're not just managing a gut condition; you're managing a condition that intersects with every aspect of your female biology and social experience. It's okay to feel overwhelmed sometimes.
The cornerstone is a healthcare team that listens to you. If your doctor dismisses your concerns about menstrual flares or sexual pain, find a new one. You deserve a provider who sees you as a whole person. Use resources from authoritative sites like the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) to stay informed and bring questions to your appointments.
Build your personal toolkit. That includes medical treatments, dietary strategies, stress-management techniques, and a strong support network. Celebrate the small victories – a good week, a successful social outing, a productive conversation with your doctor.
Finally, remember that research on sex-based differences in IBD is growing. By sharing your experiences (if you feel comfortable), you contribute to a better understanding of Crohn's disease in women. You are the expert on your own body. Pair that expertise with knowledgeable medical care, and you can build a full, vibrant life, even with Crohn's as a companion on the journey.
POST A COMMENT