Your Guide to Contraception Options: Choosing the Best Method for You
Let's cut to the chase. Choosing a birth control method isn't about finding the "best" one universally. It's about finding the best one for you, right now. Your body, your lifestyle, your future plans, your budget—they all matter. I've seen too many friends stick with a method that makes them miserable because they think it's their only option, or worse, abandon contraception altogether out of frustration.
The landscape has changed. It's not just about the pill versus condoms anymore.
Your Quick Navigation Guide
Why Getting This Choice Right Matters More Than You Think
Think of contraception as a tool. You wouldn't use a sledgehammer to hang a picture frame. Picking the wrong tool for the job leads to frustration, damage, and giving up entirely.
The goal isn't just to prevent pregnancy. It's to do so in a way that fits seamlessly into your life, supports your health, and aligns with your goals. A method that causes constant side effects or anxiety isn't sustainable. That's when people start skipping doses, taking chances, or just throwing their hands up.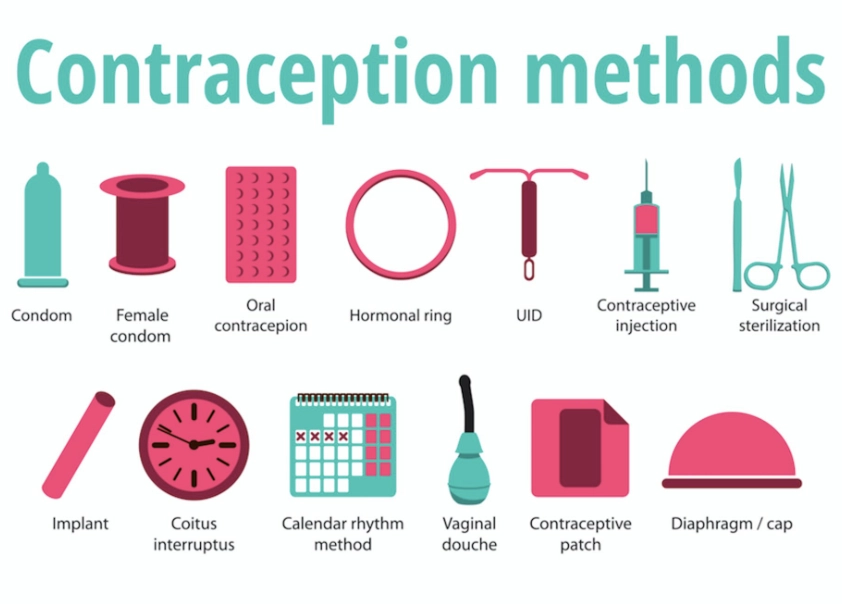
Key Insight: The most common mistake I see? People choose based on a friend's recommendation or the first thing a busy doctor mentions, without a real conversation about their daily reality. A method requiring perfect daily timing is a disaster for someone with a chaotic schedule or ADHD. An upfront cost can be a barrier, even if it saves money long-term.
This decision has weight. It affects your physical health, your mental well-being, your relationship dynamics, and your financial planning. Let's get into the specifics so you can own this choice.
The Full Menu: A Breakdown of Every Contraception Method
We'll group them by how they work and how you use them. Forget the textbook categories for a second.
Hormonal Methods (The Regulators)
These work by releasing synthetic hormones (estrogen and/or progestin) that primarily prevent ovulation. They also thicken cervical mucus and thin the uterine lining.
- The Pill: The classic. Taken daily. Offers cycle control, can help with acne and heavy periods. But it demands consistency. A weekend trip where you forget your pack can mess things up.
- The Patch: A sticker you change weekly. Good if you hate pills. Can be visible and may not stick well in humid climates or with certain skin types.
- The Vaginal Ring: A flexible ring you insert yourself for three weeks, remove for one. It's low-maintenance monthly. Some find insertion/removal awkward.
- The Shot (Depo-Provera): An injection every 3 months. Incredibly private and discrete. The big caveat? It can cause weight gain and bone density loss with long-term use, and it famously has a longer delay in the return of fertility after stopping.
- Hormonal IUD (Mirena, Kyleena, etc.): A tiny T-shaped device placed in your uterus by a healthcare provider. It releases a low dose of progestin locally for 3-8 years. Often makes periods much lighter or stops them altogether. The insertion process can be uncomfortable, but then you're protected for years with zero daily effort.
- Contraceptive Implant (Nexplanon): A matchstick-sized rod placed under the skin of your upper arm. Works for up to 5 years. The most effective method because you literally cannot mess it up. Side effects can include irregular bleeding, which is its biggest drawback for some.

Non-Hormonal & Barrier Methods
For those who want or need to avoid hormones entirely.
- Copper IUD (Paragard): The only non-hormonal, long-acting option. Works for up to 10-12 years by releasing copper ions that are toxic to sperm. No hormones mean no systemic side effects. The trade-off? It can make periods heavier and more crampy, especially for the first 6 months.
- Condoms (External & Internal): The only method that also protects against STIs. Essential for new or non-monogamous partners. Effectiveness hinges entirely on correct, every-time use. "We'll just pull out" is not a backup plan.
- Diaphragm/Cervical Cap: A dome-shaped silicone cup inserted before sex to cover the cervix. Used with spermicide. Requires planning, fitting by a doctor, and comfort with insertion.
- Spermicide: Chemicals that immobilize sperm. Available as foam, film, suppositories. Very low effectiveness alone, best paired with a barrier method.
Permanent Methods
For those absolutely certain they never want biological children.
- Tubal Ligation ("getting your tubes tied"): A surgical procedure to block or cut the fallopian tubes. It's permanent and very difficult/expensive to reverse.
- Vasectomy: A much simpler, less invasive outpatient procedure for male partners. It's more effective, cheaper, and safer than female sterilization. Reversal is possible but not guaranteed.
The Hard Numbers: Effectiveness Compared
This is where people get tripped up. You'll see two numbers: "perfect use" and "typical use." Perfect use is in a lab. Typical use is in real life, with forgotten pills, condom mishaps, and late shots. Always look at the typical use percentage. It tells the real story.
| Method | Typical Use Effectiveness* | Key Consideration |
|---|---|---|
| Implant, IUDs (Hormonal & Copper) | Over 99% | "Set and forget." Highest real-world protection. |
| Sterilization (Vasectomy/Tubal) | Over 99% | Permanent. Consider it irreversible. |
| The Shot (Depo-Provera) | 96% | Requires getting shots on time every 3 months. |
| Pill, Patch, Ring | 91-93% | User-dependent. Consistency is everything. |
| Condoms (Male) | 87% | STI protection. Must be used correctly every time. |
| Fertility Awareness Apps/Methods | 76-88% | Requires rigorous daily tracking and cycle regularity. |
| Spermicide Alone | 72-82% | Very high failure rate. Use with a barrier. |
*Data synthesized from the U.S. Centers for Disease Control and Prevention (CDC) and Planned Parenthood. Effectiveness = percentage of women not experiencing a pregnancy in the first year of use.
See the gap? The pill is 99% effective in theory, but in practice, it drops to 93%. That 6% gap represents a lot of real-world surprises. LARCs (Long-Acting Reversible Contraceptives like IUDs and the implant) bridge that gap because they remove human error.
How Do I Choose the Right Contraception Option?
Don't start with the list. Start with yourself. Grab a notepad and ask these questions.
1. What's my health profile? Do you have a history of blood clots, migraines with aura, or certain cancers? These can rule out estrogen-containing methods (the pill, patch, ring). Smoking and age over 35 also factor in. The WHO Medical Eligibility Criteria is what doctors use—be your own advocate.
2. What's my lifestyle really like? Be honest.
- Are you organized enough for a daily pill at roughly the same time?
- Do you travel frequently across time zones?
- Do you want your partner involved (like condoms) or prefer a completely private method?
- Is an upfront cost (IUD/implant) a deal-breaker, even if it's cheaper per year?
3. How do I feel about my period? Some love the monthly confirmation, others dread it. Hormonal IUDs, the implant, and some pills can lighten or eliminate periods. The copper IUD often does the opposite.
4. What's the timeline? Are you spacing kids? Done having kids? Not sure if you ever want them? This is the biggest driver.
- Not sure / years away: LARCs (IUD, implant) are gold standard. Reversible, long-term, top effectiveness.
- Within 1-2 years: Shorter-term hormonals (pill, ring, patch) or barriers if you're highly motivated.
- Never want pregnancy: Consider permanent sterilization (vasectomy/tubal).
5. What are my deal-breakers? Weight gain? Acne? Mood swings? Needing to see a doctor for removal? Write them down.
Take this list to your appointment. A good provider (at a clinic like Planned Parenthood, your OB/GYN, or a family doctor) will discuss these points with you, not just hand you a sample pack of pills.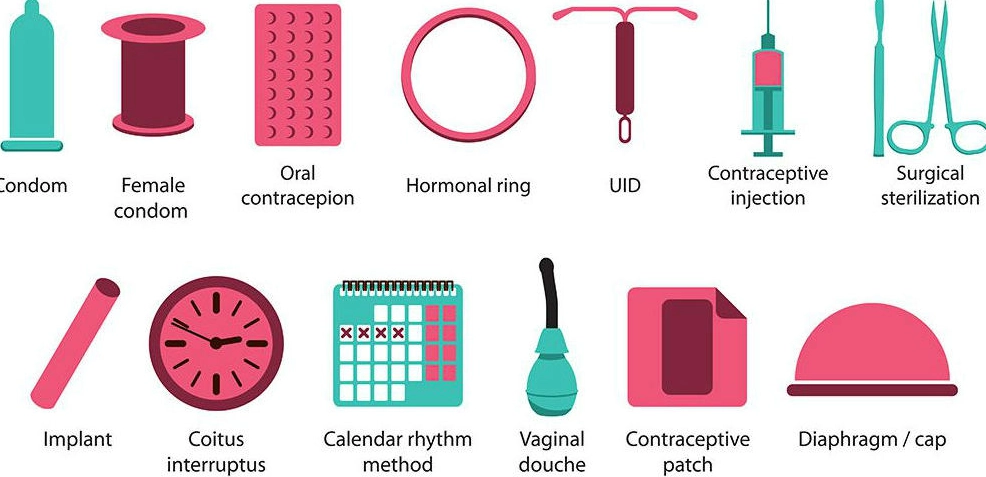
Your Top Questions, Answered Honestly
The right contraception should feel like a tool that empowers you, not a burden you tolerate. It might take one conversation, or it might take trying a couple of methods to find your fit. That's normal. Use the questions and breakdowns here to walk into that conversation informed and ready to advocate for the option that truly fits your life.
POST A COMMENT