Digestive Issues in Women: Causes, Symptoms, and Solutions
If you're a woman who feels like your stomach has a mind of its own, you're not imagining it. Bloating that comes and goes with your cycle, constipation that flares up for no obvious reason, or a diagnosis of IBS that feels vague and frustrating—these are incredibly common experiences. But here's what many articles miss: women's digestive systems operate on a unique physiological stage set by hormones, anatomy, and often, the sheer weight of societal stress.
It's not just about what you eat. It's about when you eat, how you manage stress, and what your hormones are doing at any given moment. Treating a woman's gut like a man's is a fundamental error. The solutions are more nuanced.
What You'll Find in This Guide
The Most Common Digestive Issues Women Face
While men and women share many gut problems, the prevalence and presentation differ sharply. Women are diagnosed with Irritable Bowel Syndrome (IBS) at nearly twice the rate of men. We also report more bloating, constipation, and functional dyspepsia.
A quick note on "functional" disorders: Terms like IBS or functional dyspepsia mean tests show no structural damage (like an ulcer), but the gut isn't working correctly. This doesn't mean the symptoms aren't real. It means the problem is in the function—the motility, sensitivity, or brain-gut communication.
Let's break down the big ones:
Irritable Bowel Syndrome (IBS)
The classic chameleon. It's not one condition but a cluster of symptoms: abdominal pain linked to bowel movements, along with changes in stool frequency or form. Women are more likely to have IBS with constipation (IBS-C) or the mixed type (IBS-M). The pain can be debilitating, often centered in the lower abdomen.
Bloating and Distension
This is the one that drives so many women crazy. That feeling of tightness, fullness, and your clothes not fitting by the end of the day. For some, it's purely sensory (you feel bloated). For others, there's visible distension (your belly actually protrudes). It's a hallmark of IBS but can stand alone.
Chronic Constipation
Defined as having fewer than three bowel movements per week, with stools that are hard, lumpy, and difficult to pass. Women's colons have longer transit times, meaning things move slower. Add in pelvic floor dysfunction (which is rarely discussed but common postpartum), and you have a mechanical problem on top of a motility one.
GERD and Heartburn
Pregnancy is a major trigger due to progesterone relaxing the lower esophageal sphincter and the growing uterus pressing on the stomach. But even outside pregnancy, women are susceptible, particularly if they have a hiatal hernia.
| Issue | Key Symptoms | Common Female-Specific Triggers |
|---|---|---|
| IBS-C (Constipation-Predominant) | Abdominal pain, bloating, infrequent/hard stools | High progesterone phase (post-ovulation), stress, low fiber intake |
| Functional Bloating | Feeling of fullness, tightness, visible distension | Menstrual cycle, high-FODMAP foods, swallowing air (aerophagia) when anxious |
| Functional Dyspepsia | Early fullness, upper abdominal pain/burning, nausea | Stress, eating too quickly, certain medications (NSAIDs) |
The Root Causes: More Than Just Food
You've probably tried cutting out gluten or dairy. Maybe it helped a bit, but the problem returned. That's because the engine driving women's digestive issues often has multiple fuel lines.
The Hormone Rollercoaster
Estrogen and progesterone aren't just for reproduction; they have receptors all over your gastrointestinal tract. Progesterone, in particular, is a smooth muscle relaxant. In the second half of your cycle, it slows everything down. Food moves more sluggishly through the intestines, leading to gas buildup, bloating, and constipation. This is why so many women feel their worst in the week before their period.
Estrogen influences gut sensitivity and serotonin levels (95% of your body's serotonin is in your gut!). Fluctuations during perimenopause can suddenly trigger new digestive woes.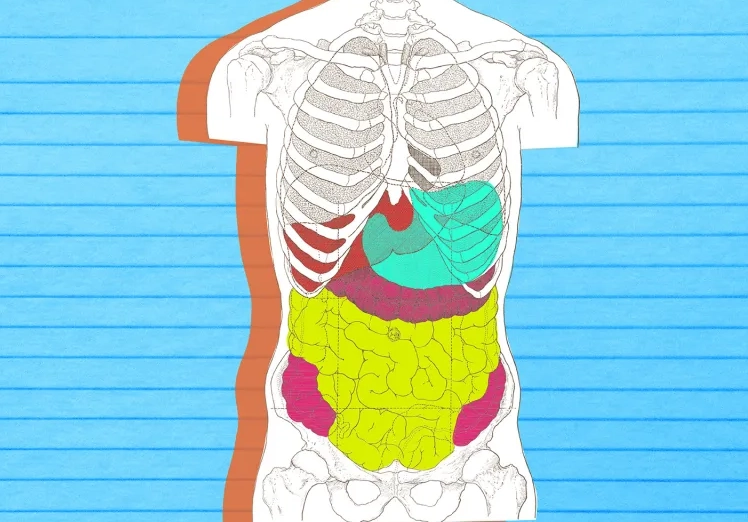
The Stress-Gut Axis (It's Real)
Chronic stress floods your system with cortisol. This hormone can increase gut permeability ("leaky gut"), alter motility, and change your microbiome. Women often juggle multiple roles, leading to chronic, low-grade stress that the gut feels acutely. The brain talks to the gut via the vagus nerve, but in conditions like IBS, this communication goes haywire—the gut becomes hypersensitive, interpreting normal movements as painful.
Anatomy Matters
A woman's pelvic cavity is more crowded. The colon has to share space with the uterus and ovaries. During menstruation or with conditions like endometriosis (which can implant on the bowel itself), this proximity causes direct irritation and symptoms that mimic IBS.
The Microbiome Mystery
Early research suggests men and women have different gut bacteria compositions, possibly influenced by hormones. This may affect how we metabolize food, produce gas, and respond to inflammation.
A Practical Guide to Managing Your Symptoms
Forget the one-size-fits-all cleanse. Effective management is about becoming a detective of your own body.
1. Track Your Cycle and Your Meals
Use an app or a simple notebook. For two months, note:
- Where you are in your menstrual cycle.
- What you eat and when.
- Your stress levels (scale of 1-10).
- Your symptoms (bloating, pain, stool type).
You might find your "trigger foods" are only problematic during your luteal phase (after ovulation). That changes the strategy completely—instead of permanent elimination, you might just modify your diet for that one week.
2. Rethink Your Approach to Fiber
"Eat more fiber" is standard advice, but it backfires for many women with IBS. The key is soluble vs. insoluble fiber.
- Soluble Fiber (dissolves in water): Acts like a gel, slowing digestion. Good for both diarrhea and constipation. Sources: Oats, psyllium husk (like Metamucil), chia seeds, apples (without skin), carrots.
- Insoluble Fiber (doesn't dissolve): Adds bulk, can speed transit. Can worsen diarrhea and bloating in sensitive guts. Sources: Wheat bran, whole grains, many raw vegetables, nuts.
Start with soluble fiber. Add a teaspoon of psyllium husk to water daily, and increase slowly over weeks.
3. Master Stress Management (Not Just Meditation)
It's not about eliminating stress; it's about changing your body's response to it. Diaphragmatic breathing (deep belly breathing) for 5 minutes, twice a day, directly stimulates the vagus nerve, activating the "rest and digest" system. It's a physical reset button for your gut. Regular, gentle exercise like walking or yoga is also proven to improve IBS symptoms more effectively than vigorous cardio for some.
4. The Low-FODMAP Diet: A Tool, Not a Lifestyle
FODMAPs are fermentable carbs that can draw water into the gut and feed gas-producing bacteria. A strict low-FODMAP diet should be done with a dietitian's guidance for only 2-6 weeks. The goal is to identify triggers, not live in restriction forever. Most people react to only one or two FODMAP groups (e.g., fructans in wheat/onions, or lactose).
When It's Time to See a Doctor
Self-management has limits. Don't suffer in silence or self-diagnose with Dr. Google. See a gastroenterologist if you experience:
- Unexplained weight loss.
- Blood in your stool (bright red or dark/black).
- Severe, persistent pain that wakes you up at night.
- Difficulty swallowing or persistent vomiting.
- Family history of ovarian, colon, or stomach cancer, or inflammatory bowel disease (IBD).
- New symptoms starting over age 50.
Even without these red flags, if symptoms control your life, seek help. A good doctor will work to rule out celiac disease (via blood test), IBD, SIBO (Small Intestinal Bacterial Overgrowth), and pelvic floor disorders.
Your Questions, Answered
The path to a happier gut isn't about finding a single miracle cure. It's about understanding the unique interplay of hormones, nerves, microbes, and life in a woman's body. Start with observation, be kind to yourself, and don't hesitate to build a healthcare team that takes your symptoms seriously.
POST A COMMENT