Bacterial Vaginosis: Symptoms, Treatments, and How to Prevent It
Quick Navigation
- So, What Exactly Are the Signs of Bacterial Vaginosis?
- Unpacking the Causes: What Throws Your Vaginal Flora Off Balance?
- Getting a Diagnosis: Don't Play Guessing Games
- Bacterial Vaginosis Treatment Options: What's on the Menu?
- Beyond Antibiotics: Probiotics and the Recurrence Puzzle
- Bacterial Vaginosis vs. Yeast Infection: The Ultimate Showdown
- The Bigger Picture: Why Treating BV Matters
- Your Action Plan: Prevention and Living with a Happy Vagina
Let's talk about something that's incredibly common but still wrapped in a weird silence. Bacterial vaginosis. If you've ever had it, you know the drill. That off smell, the weird discharge, the nagging worry that something's wrong. And if you haven't, well, chances are you might at some point. It's that prevalent.
I remember the first time I Googled my symptoms. The information was all over the place. Was it a yeast infection? An STD? Was I just unclean? Spoiler alert: it was none of those. It was bacterial vaginosis, a simple imbalance in the vaginal flora. But the confusion and anxiety were very real. That's why I wanted to put this together – to cut through the noise and give you the straight facts, the kind I wish I'd found.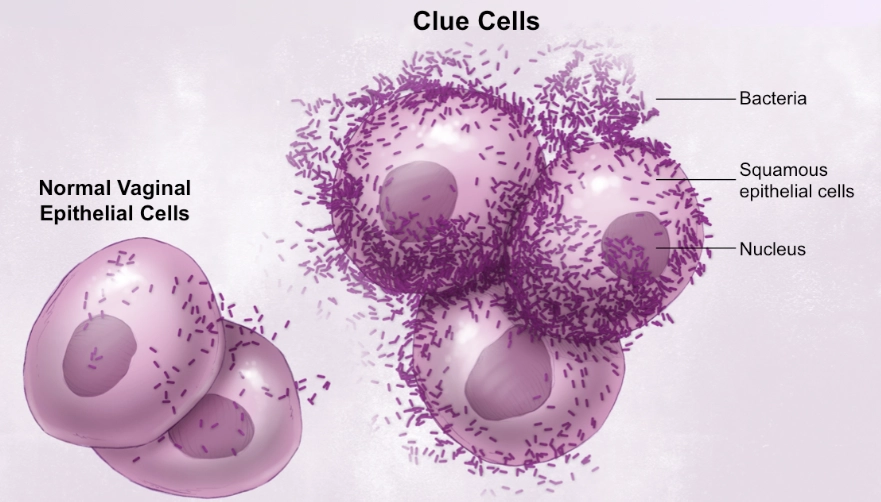
Quick Take: Bacterial vaginosis (BV) isn't an infection you "catch" from someone else like an STD. It's more like your vaginal garden's ecosystem got out of whack. The good bacteria (mainly Lactobacilli) take a hit, and other bacteria that are usually present in small numbers start to overgrow. That's the core of the issue.
So, What Exactly Are the Signs of Bacterial Vaginosis?
This is where things get tricky. Up to half of all women with BV don't have any symptoms at all. Zero. They might only find out during a routine pap smear. For the rest of us, the signs can be subtle or pretty obvious.
The classic symptom, the one that sends most people searching, is a thin, grayish-white discharge. It often has a distinct fishy odor, especially after sex or during your period. That's because semen and menstrual blood have a higher pH, which can trigger the odor-causing chemicals produced by the BV-associated bacteria.
Other symptoms can include burning when you pee (which is why it's often confused with a UTI) and sometimes itching around the outside of the vagina. But here's the key difference from a yeast infection: the itching with BV is usually milder, and the discharge is totally different. Yeast infection discharge is typically thick, white, and clumpy (like cottage cheese) and doesn't usually have a strong odor.
Heads up: That fishy odor is a major clue. If you notice it, particularly after intercourse, it's a strong indicator that you might be dealing with bacterial vaginosis and not something else. Don't just assume it's a yeast infection and grab the over-the-counter cream – it won't work and might make things more uncomfortable.
Why does this happen? What causes this bacterial imbalance in the first place?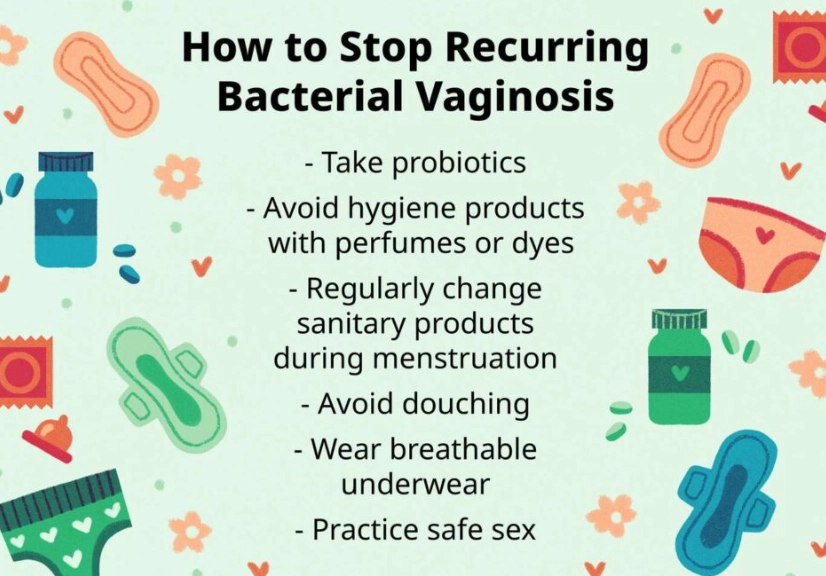
Unpacking the Causes: What Throws Your Vaginal Flora Off Balance?
Doctors don't always have a single, clear answer for why one person gets BV and another doesn't. It's not about being "dirty." In fact, douching is a major risk factor because it washes away the protective good bacteria. So please, stop douching. Your vagina is self-cleaning.
The thinking now is that anything that changes the natural acidity (pH) of the vagina can open the door for BV. Here's a rundown of the common triggers:
- New or Multiple Sexual Partners: This is a big one. It's not that BV is an STD, but having sex, especially with a new partner or multiple partners, can introduce new bacteria and alter your vaginal pH. It's more about the activity than the transmission of a specific bug.
- Lack of Lactobacilli: Some women naturally have lower levels of these protective good bacteria, making them more susceptible.
- Smoking: Yep, another reason to quit. Smoking is linked to a higher incidence of BV.
- Your Period: The blood can raise the vaginal pH, creating a more friendly environment for the BV bacteria.
- IUDs: Some studies show a possible link between IUD use and a higher risk of BV, though the data isn't conclusive. The string might act as a pathway for bacteria.
It's frustrating, isn't it? Sometimes it feels like just being a woman and having a vagina is a risk factor. The reality is that the vaginal microbiome is a delicate balance, and modern life throws a lot at it.
Getting a Diagnosis: Don't Play Guessing Games
If you suspect you have bacterial vaginosis, the best thing you can do is see a healthcare provider. This isn't something you should definitively diagnose yourself. Why? Because the symptoms overlap with other conditions like yeast infections, trichomoniasis (an STD), and even some normal variations.
Your doctor or nurse will usually do a simple pelvic exam. They'll look for the characteristic discharge and check your vaginal pH (which is elevated in BV). They might also take a sample of the discharge, put it on a slide, add a drop of potassium hydroxide (KOH), and sniff. Sounds weird, but it's called the "whiff test" – if a strong fishy odor is released, it points to BV. Finally, they might look at the sample under a microscope to see if the "clue cells" (vaginal cells covered with BV bacteria) are present.
According to the U.S. Centers for Disease Control and Prevention (CDC) treatment guidelines, a diagnosis of bacterial vaginosis is typically made when at least three of the following four criteria (called Amsel's criteria) are met:
- Thin, white, homogeneous discharge.
- Clue cells on microscopy.
- Vaginal fluid pH > 4.5.
- A positive whiff test.
Pro Tip: Before your appointment, avoid vaginal intercourse, douching, or using any vaginal creams or medications for at least 24-48 hours. These can mess with the test results and make it harder to get an accurate diagnosis.
Okay, so you've been diagnosed. Now what?
Bacterial Vaginosis Treatment Options: What's on the Menu?
Here's the good news: bacterial vaginosis is usually easy to treat with antibiotics. The bad news? Recurrence is super common. Like, really common. Up to 50% of women see symptoms come back within a year. That's the frustrating part that standard treatment doesn't always address.
The main goal of treatment is to knock back the overgrown bacteria and, hopefully, let the good Lactobacilli reclaim their territory. Here are the standard first-line treatments recommended by health authorities like the World Health Organization (WHO) and the CDC.
| Medication | Form | How to Take It | Key Points & My Take |
|---|---|---|---|
| Metronidazole | Oral Pill | 500 mg twice daily for 7 days. | The gold standard. Very effective. Big warning: NO ALCOHOL while taking it and for at least 48 hours after. It causes a severe reaction (nausea, vomiting, flushing). Personally, I found the side effects (metallic taste, potential stomach upset) a bit rough. |
| Metronidazole Gel (0.75%) | Vaginal Gel | One applicatorful (5g) intravaginally once daily for 5 days. | My preferred method. Fewer systemic side effects than the pill. You can usually drink alcohol with this form (but always check with your pharmacist!). Less mess than the cream options, in my experience. |
| Clindamycin Cream (2%) | Vaginal Cream | One applicatorful intravaginally at bedtime for 7 days. | A good alternative for those allergic to metronidazole. Important: Clindamycin is oil-based and can weaken latex condoms and diaphragms for several days after treatment. Something to keep in mind. |
| Tinidazole | Oral Pill | 2g single dose OR 1g daily for 5 days. | Similar to metronidazole but sometimes better tolerated. The same strict no-alcohol rule applies. It's often used for recurrent or stubborn cases. |
You'll notice these are all antibiotics. They work, but they're a bit of a blunt instrument. They kill the bad guys but can also take out some of the good guys you're trying to repopulate. That's where the recurrence problem often starts.
Beyond Antibiotics: Probiotics and the Recurrence Puzzle
This is the million-dollar question. How do you stop bacterial vaginosis from coming back? The medical community is still figuring this out, but the focus has shifted heavily towards vaginal microbiome health.
Probiotics, both oral and vaginal, are a huge area of interest. The idea is to directly replenish the Lactobacilli. Some studies show promise, especially for women with recurrent BV. Look for strains specifically studied for vaginal health, like Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14. A resource like Harvard Health Publishing often reviews the evidence on this.
Other things people try include boric acid suppositories (which must be prescribed or compounded by a pharmacist – never ingest boric acid!) and maintaining a lower-sugar diet. The evidence for these is more anecdotal, but anecdotally, many women swear by them as part of a maintenance routine.
The truth is, managing recurrent BV is often about a combination approach: treating the acute episode with prescribed antibiotics and then working on long-term balance with probiotics and lifestyle tweaks. It's more of a marathon than a sprint.
Bacterial Vaginosis vs. Yeast Infection: The Ultimate Showdown
This is probably the most common point of confusion. They feel similar in some ways but are completely different beasts. Getting this wrong means wasting money on the wrong treatment and prolonging your discomfort.
Let's break it down simply:
- Discharge: BV = thin, gray/white, watery. Yeast = thick, white, clumpy (cottage cheese).
- Odor: BV = fishy, strong, especially after sex. Yeast = usually no odor, or a mild bread-like yeast smell.
- Itching/Burning: BV = possible mild external itching, burning with urination. Yeast = INTENSE itching and irritation, both inside and out, often with significant swelling and redness.
- Cause: BV = bacterial overgrowth (anaerobes). Yeast = fungal overgrowth (Candida albicans).
- Treatment: BV = requires prescription antibiotics (metronidazole, clindamycin). Yeast = often treatable with OTC antifungals (miconazole, clotrimazole).
The Bigger Picture: Why Treating BV Matters
You might think, "If it's not an STD and sometimes has no symptoms, why bother treating it?" That's a fair question, but there are important health reasons.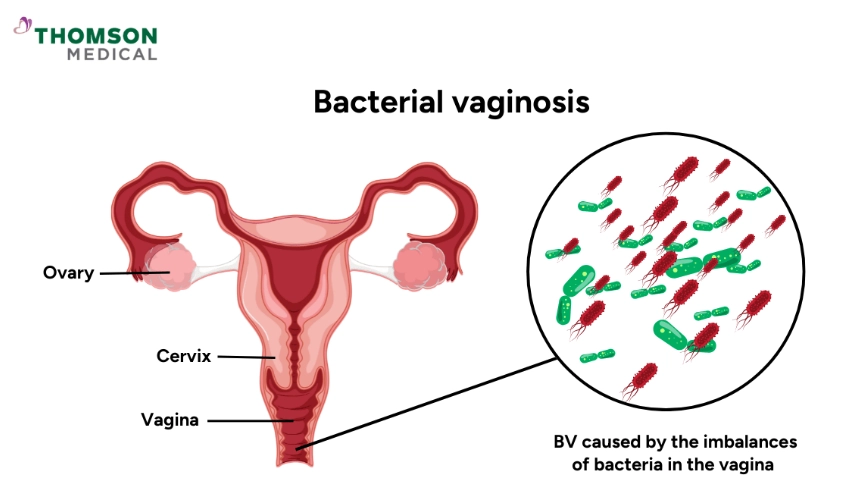
Having bacterial vaginosis changes the vaginal environment in ways that can make you more susceptible to other issues. It's associated with an increased risk of:
- Sexually Transmitted Infections (STIs): Including HIV, chlamydia, gonorrhea, and herpes. The imbalance and inflammation might make it easier for these pathogens to take hold.
- Pelvic Inflammatory Disease (PID): An infection of the reproductive organs that can lead to chronic pain and infertility.
- Pregnancy Complications: This is a major one. In pregnant women, BV is linked to a higher risk of preterm delivery, low birth weight, and miscarriage.
- Post-Surgical Infections: If you're having a procedure like a hysterectomy or abortion, having BV increases the risk of developing an infection afterwards.
So, while it might seem like just a nuisance, treating bacterial vaginosis is an important part of your overall reproductive and sexual health.
Your Action Plan: Prevention and Living with a Happy Vagina
Since recurrence is the name of the game for many, prevention is key. It's about creating an environment where the good bacteria thrive. Think of it as gardening.
Here's my personal ranking of the most effective strategies, based on evidence and what's worked for me and others I've talked to:
- Stop Douching. Forever. Your vagina has its own elegant cleaning system. Douching disrupts it, plain and simple.
- Consider Probiotics. Especially around periods of higher risk (after antibiotics, during periods of stress, or if you're sexually active with new partners). Look for the specific vaginal health strains mentioned earlier.
- Wipe Front to Back. Always. This prevents bacteria from the anal area from getting near the vagina.
- Choose Breathable Underwear. Cotton is your friend. Avoid tight, synthetic fabrics that trap moisture.
- Be Mindful with Sex. Using condoms can help maintain pH balance. Urinating after sex is always a good practice to help prevent UTIs, which can be confused with BV symptoms.
- Manage Stress. This one is hard, but chronic stress impacts your entire body, including your immune system and potentially your microbiome.
It's not about being perfect. It's about making small, sustainable choices that support your body's natural balance.
- Extended or Suppressive Therapy: Taking a lower dose of antibiotics (like metronidazole gel) twice a week for several months to prevent overgrowth.
- Using a Different Antibiotic: Switching from metronidazole to clindamycin or tinidazole.
- Combination Therapy: Combining an antibiotic treatment with a course of specific probiotics.
- Investigating Underlying Causes: In rare cases, recurrent BV can be a sign of another issue like biofilm formation (where bacteria create a protective layer that antibiotics can't penetrate easily).
It's a process of trial and error, and it requires patience and a good partnership with your doctor.
Look, dealing with bacterial vaginosis, especially the recurrent kind, can be draining. It can affect your self-esteem, your sex life, and just your general peace of mind. The information out there is often conflicting or fear-based.
My hope is that this gives you a clear, practical, and human roadmap. You now know what bacterial vaginosis is, how to spot it, how it's properly diagnosed, and what the treatment landscape looks like. You understand why it's more than just a nuisance and have some solid strategies to try and prevent it from becoming a regular, unwelcome guest.
Remember, your body is always trying to find balance. Sometimes it just needs a little help. Don't suffer in silence or feel ashamed. It's a common medical condition, full stop. Talk to your doctor, advocate for yourself if the first treatment doesn't stick, and know that with the right approach, you can manage this and get back to feeling like yourself.
POST A COMMENT