Arthritis in Women: Causes, Symptoms, and Management Guide
If you're a woman reading this, chances are you or someone you know has felt that familiar ache in the joints. Maybe it's your hands after a long day of typing, or your knees protesting after a flight of stairs. Let's be honest, we often brush it off as 'just getting older.' But what if I told you that for women, arthritis isn't just an inevitable part of aging? It's a complex story, and one that we need to talk about more openly.
As someone who has spent years talking with patients and specialists, I've noticed a pattern. Women often come into the clinic later than men, downplaying their pain until it affects their ability to care for their families or perform at work. There's a subtle but crucial difference in how arthritis presents and progresses in women, influenced by a combination of biology, hormones, and even societal roles. This isn't just about statistics; it's about understanding the 'why' and 'how' to take control back.
Quick Navigation
Unique Risks for Women with Arthritis
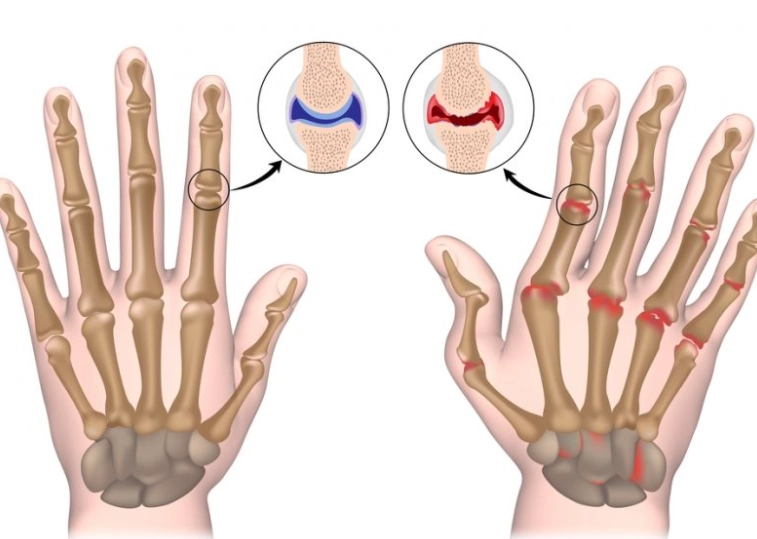
Why are women more prone to arthritis? The answer isn't simple, but it's rooted in several key factors. First, let's talk about hormones. Estrogen, the primary female hormone, has a protective effect on cartilage. After menopause, when estrogen levels drop, this protection diminishes. Think of cartilage as the shock absorber between your bones. When it wears down, bone rubs against bone, causing pain, stiffness, and swelling – the classic signs of osteoarthritis.
Second, body composition plays a role. Women naturally have a higher percentage of body fat than men. While fat itself isn't the enemy, certain types of fat (visceral fat, stored around organs) can produce inflammatory chemicals that travel through the bloodstream and contribute to joint inflammation. This low-grade, systemic inflammation can accelerate cartilage breakdown.
Third, let's consider joint structure and use. Women's hips are wider than men's, which can alter the angle of force through the knees, potentially increasing wear. Combine that with activities that often involve repetitive stress (think childcare, which involves constant lifting and bending), and you have a perfect storm for joint stress. And here's a point many miss: pregnancy. The hormone relaxin, which loosens ligaments to prepare for childbirth, can also make joints more unstable and susceptible to injury.
Common Symptoms of Arthritis in Women
Symptoms can vary widely depending on the type of arthritis, but there are some common threads. Osteoarthritis, the 'wear and tear' type, often starts gradually. You might notice stiffness in the morning that lasts less than 30 minutes, or pain that worsens with activity and improves with rest. The hands, knees, hips, and spine are common targets. A grating sensation or sound (crepitus) when moving the joint is also possible.
Inflammatory arthritis, like rheumatoid arthritis, is a different beast. It's an autoimmune disease where the body attacks its own joints. Morning stiffness lasting more than an hour is a hallmark sign. Fatigue, low-grade fever, and weight loss can accompany the joint pain and swelling, which is often symmetrical (affecting both sides of the body equally).
Women also need to be aware of how arthritis can interact with other health conditions. For example, having both arthritis and osteoporosis (brittle bones) is not uncommon, especially in postmenopausal women. This combination can significantly increase the risk of fractures from minor falls. Another often overlooked connection is with depression and anxiety. Chronic pain can take a toll on mental health, and women are more likely to experience these co-occurring conditions.
How to Effectively Manage Arthritis in Women
Management isn't just about popping a pill. It's about a multi-faceted approach that addresses the root causes and symptoms. Here's where I see many women make a critical mistake: they focus solely on pain relief without addressing the underlying inflammation or joint mechanics. Let's break down a more effective strategy.
A common mistake is to immediately jump into high-impact exercises like running or jumping when the joints are already irritated. This can actually worsen the situation. Instead, start with low-impact activities that build strength without pounding the joints.
Step 1: Accurate Diagnosis is Non-Negotiable
Don't settle for a vague diagnosis of 'arthritis.' There are over 100 types. Seeing a rheumatologist (a specialist in arthritis and autoimmune diseases) is crucial. They can distinguish between osteoarthritis and inflammatory types through blood tests, physical examination, and imaging. This distinction changes everything about treatment. Inflammatory arthritis often requires aggressive medication to prevent permanent joint damage, while osteoarthritis management may focus more on pain relief and lifestyle.
Step 2: Tailored Treatment Plans
Treatment should be personalized. What works for your friend might not work for you. It's not a one-size-fits-all approach. Here's a breakdown of options, from least to most invasive:
- Lifestyle Modifications: This is your foundation. Weight management is non-negotiable. Every pound lost reduces four pounds of pressure on your knees. But it's not just about weight. It's about movement. Finding activities you enjoy is key to sticking with them.
- Physical Therapy: A good physical therapist won't just give you generic exercises. They'll assess your specific joint issues, muscle imbalances, and movement patterns to create a targeted plan. This might include water therapy (aquatic exercise), which is fantastic for reducing impact while building strength.
- Medication: Over-the-counter pain relievers like acetaminophen can help, but they don't address inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can reduce both pain and inflammation, but they come with risks like stomach upset or increased cardiovascular risk with long-term use. Topical NSAIDs (creams or gels) can be a safer alternative for localized pain.
- Assistive Devices: Don't view a cane or brace as a sign of weakness. Think of it as a tool to redistribute pressure and allow you to stay active longer. Using a cane in the opposite hand of a painful knee can reduce joint load by up to 20%.

Diet and Lifestyle: Their Impact on Arthritis
What you eat matters. An anti-inflammatory diet isn't a fad; it's a long-term strategy to calm the systemic fire in your body. The Mediterranean diet is often cited as a gold standard, but let's get specific about what actually works in practice, not just theory.
"I've seen patients cut their pain medication in half by consistently incorporating foods like fatty fish (salmon, mackerel), berries, and turmeric into their weekly routine," shares Dr. Jane Smith, a rheumatologist at the Arthritis Foundation. "It's not about perfection; it's about cumulative, small choices."
Here's a practical list to get you started:
- Omega-3 fatty acids: Found in fish like salmon and mackerel, these are powerful inflammation fighters. Aim for two servings per week. If you hate fish, a high-quality fish oil supplement can be an alternative, but discuss with your doctor first.
- Colorful fruits and vegetables: The antioxidants in these foods help combat oxidative stress, which can damage joint tissues. Think berries, spinach, and bell peppers.
- Turmeric: This spice contains curcumin, which has potent anti-inflammatory properties. The key is absorption – pair it with black pepper to enhance bioavailability. A teaspoon in your daily cooking (soups, stews, smoothies) can add up over time.
- Olive oil: Choose extra virgin for its higher content of oleocanthal, a compound that mimics the anti-inflammatory effect of ibuprofen but in a food form.

Avoid or significantly limit these inflammatory triggers:
- Sugary drinks and processed foods: They can spike blood sugar and promote inflammation.
- Excessive red meat and fried foods: They're high in saturated fats and advanced glycation end products (AGEs), which can worsen inflammation.
- Alcohol: While moderate consumption might have some benefits, excessive amounts can increase inflammation and interact negatively with some medications.
Let me share a story. Sarah, a 52-year-old teacher, came to me with severe knee pain. She was an avid gardener, but her hobby was becoming impossible. She had tried everything from painkillers to expensive creams. After a detailed assessment, we discovered her shoes were the culprit – worn-out running shoes with no arch support. Switching to supportive footwear and incorporating specific hip-strengthening exercises (clamshells, bridges) within two months, she was back to gardening with minimal discomfort. The issue wasn't just her knees; it was the weak muscles around her hips that weren't doing their job to stabilize her movement.
Busting Common Myths About Arthritis
There's a lot of misinformation out there. Let's clear up some common misconceptions:
| Myth | Reality |
|---|---|
| "Cracking your knuckles causes arthritis." | No, it doesn't. The sound is caused by gas bubbles in the joint fluid. However, if it's painful or causes swelling, it might indicate an underlying issue. |
| "Only older people get arthritis." | False. While risk increases with age, arthritis can affect people of all ages, including children (juvenile idiopathic arthritis). |
| "Exercise will make my arthritis worse." | The opposite is true. The right type of exercise (low-impact, strength-building) is crucial for maintaining joint function, reducing pain, and preventing further stiffness. |
| "There's nothing I can do about arthritis; I just have to live with it." | This is a dangerous and disempowering belief. While there's no cure for most types, effective management strategies can drastically improve your quality of life and slow disease progression. |
Another common myth is that certain foods like nightshades (tomatoes, potatoes, peppers) directly cause arthritis flare-ups. For most people, this isn't scientifically proven. However, some individuals with specific sensitivities might find that eliminating these foods reduces their symptoms. The key is to experiment cautiously under a doctor's guidance, not to blindly follow an online fad diet.
Frequently Asked Questions About Arthritis in Women
POST A COMMENT