Pap Smear Test: A Complete Guide to What It Is, Why You Need It, and What Results Mean
Let's be real. The words "Pap smear test" don't exactly spark joy. For most of us, it brings to mind a cold exam room, awkward positions, and a vague sense of anxiety about what the doctor might find. I remember my first one. I was 21, nervous, and honestly, I had no clue what to expect beyond the basic description from a pamphlet. I spent more time worrying about the unknown than understanding why it was so important.
That's why I'm writing this. Not as a medical professional (I'm not one), but as someone who's been through it and has talked to countless friends about their experiences. I've done a ton of reading from reliable sources to make sense of it all. Consider this a friendly, no-BS guide that cuts through the medical jargon and gets to the heart of what you actually want to know.
What is it, really? Why does everyone keep telling you to get one? What's the deal with the speculum? And most importantly, what do those results actually mean when they come back?
The core idea is simple: A Pap smear test (also called a Pap test) is a screening tool. Its main job is to find precancerous changes in the cells of your cervix—that's the lower, narrow end of your uterus that connects to the vagina. The genius of it is that it finds problems before they turn into cancer, when they're easiest to treat. Think of it like a very early warning system.
In This Guide
- Why Bother? The Real Reason Pap Smears Are a Big Deal
- Getting Ready: What You Should (and Shouldn't) Do
- The Step-by-Step: What Actually Happens in the Room
- Decoding Your Pap Smear Results: Don't Panic
- How Often Do You Really Need a Pap Smear Test?
- Busting the Biggest Pap Smear Myths
- Answers to Questions You're Too Embarrassed to Ask
- The Bottom Line: Your Health, Your Power
Why Bother? The Real Reason Pap Smears Are a Big Deal
You might think, "I feel fine, why do I need this?" That's the whole point. Cervical cancer is sneaky. The precancerous changes and even early cancer often have zero symptoms. None. By the time you notice something wrong, it's a much more serious situation.
The success story here is almost unbelievable. Since Pap smears became widespread, deaths from cervical cancer have dropped by more than 50% in countries with strong screening programs. That's not just a statistic—that's millions of lives. The American Cancer Society calls it one of the most effective cancer screening tests ever developed.
It's all about catching those abnormal cells early. An abnormal Pap smear result doesn't mean you have cancer. In fact, most of the time it doesn't. It's a flag that says, "Hey, let's keep an eye on this area or do a quick check to see what's up." That follow-up might be another test in a year, or a closer look with a colposcopy. It's a process.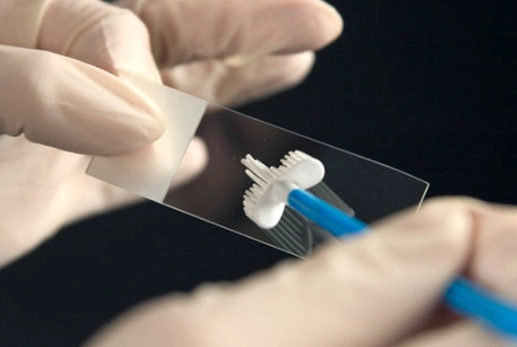
A friend of mine had an abnormal result a few years back. She was terrified, thinking the worst immediately. After a colposcopy (which she said was more uncomfortable than the Pap smear itself), they found a small area of precancerous cells and removed them right there in the office. That was it. She gets checked more frequently now, but the key is they caught it when it was 100% treatable. That experience changed how I view the test—it's not a judgment, it's a tool.
Getting Ready: What You Should (and Shouldn't) Do
Preparation isn't complicated, but getting it wrong can sometimes mess with the sample and lead to an unclear result, which means you might have to do it again. Nobody wants that.
Here’s the practical list most doctors will give you:
- Schedule wisely: Try to book your appointment for a time when you are not on your period. Heavy flow can obscure the cells. If your period comes unexpectedly, it's usually okay if it's light, but call your clinic to double-check. They see it all the time.
- The 48-hour rule: For two days before the test, avoid anything that goes into the vagina. That means no sex, no tampons, no douching (you shouldn't be douching anyway, it's not good for you!), no vaginal medicines or creams, and no spermicidal foams or jellies. This helps ensure the sample collected is just your cervical cells and not confused by other substances.
- Relaxation is key: I know, easier said than done. But being tense can make the physical part more difficult. Take some slow breaths. Remember, for your healthcare provider, this is a routine, clinical procedure they do dozens of times a week.
What about pain? For most people, a Pap smear test is more of a brief pressure or a weird sensation than actual pain. You might feel a small scrape or brush. It lasts less than a minute. If you have a history of pain during pelvic exams or conditions like vaginismus, talk to your doctor before the exam starts. They can adjust, use a smaller speculum, and go slower.
The Step-by-Step: What Actually Happens in the Room
Okay, let's walk through it. Knowing what's coming can take away a lot of the fear.
Before the Exam
You'll be asked to undress from the waist down and given a sheet or gown to cover yourself. You'll lie on the exam table on your back, usually with your feet in supports called stirrups. This position allows the doctor or nurse practitioner to see the cervix clearly. It feels exposed, but they are focused on the anatomy, not judging you.
During the Pap Smear Procedure
- The Speculum: The provider will gently insert a speculum into your vagina. This is a plastic or metal tool that holds the vaginal walls open so they can see the cervix. They often warm it up. You'll feel pressure. If it's painful, say so—they can adjust.
- The Visual Check: They'll take a quick look at your cervix and vagina to check everything looks healthy.
- The Collection: Using a small, soft brush or a spatula (or both), they will gently scrape a sample of cells from your cervix. This is the "smear" part. You might feel a quick, light scratching sensation or a tiny cramp. It's over in about 10-15 seconds. Seriously.
- Done: The speculum is removed, and that's it for the Pap. The cell sample is smeared on a glass slide or placed in a liquid preservative (a "liquid-based" Pap) and sent to a lab.
Sometimes, they'll do an HPV test at the same time, using a second brush or from the same liquid sample. HPV (human papillomavirus) is the virus that causes almost all cervical cancers. Testing for it alongside the Pap is becoming very common.
And then you get dressed.
The whole pelvic exam part, including the Pap smear test, usually takes about 5-10 minutes total. The actual cell collection is the shortest part.
Decoding Your Pap Smear Results: Don't Panic
This is where anxiety peaks. You get a letter or a portal message with terms like "ASC-US" or "LSIL." It looks like alphabet soup. Let's translate.
First, know that most Pap smear results come back as normal (often called "negative"). That means no abnormal cells were found. You're good for your next routine screening in a few years.
An abnormal result is NOT a cancer diagnosis. It means some cells on your cervix look different from normal cells. The vast majority of these changes are caused by HPV, and most HPV infections clear up on their own without ever causing problems. The abnormal cells often go away too.
| Result Term | What It Means (In Plain English) | What Usually Happens Next |
|---|---|---|
| Normal / Negative | No abnormal cells found. Great news. | Come back for your next routine screening in 3-5 years (depending on your age and history). |
| ASC-US (Atypical Squamous Cells of Undetermined Significance) |
Some cells look slightly off, but it's unclear why. This is the most common abnormal finding. | Often, the lab will automatically check the sample for HPV if they haven't already. If HPV is negative, it's likely fine. If HPV is positive, you may need a colposcopy. |
| LSIL (Low-grade Squamous Intraepithelial Lesion) |
Mild cell changes are present. Often linked to a recent HPV infection. | Since these often clear on their own, the next step might be a colposcopy or simply a repeat Pap in 6-12 months. |
| HSIL (High-grade Squamous Intraepithelial Lesion) |
More pronounced cell changes. These are more likely to develop into cancer if left untreated. | A colposcopy is almost always recommended to get a closer look and possibly take a biopsy. |
| AGC (Atypical Glandular Cells) |
Changes in the glandular cells (which are in a different part of the cervix). This is less common but needs evaluation. | Usually requires a colposcopy and possibly other tests. |
See? It's a spectrum, from "watch this" to "let's investigate further." The goal of the follow-up is to prevent anything from progressing. If a biopsy confirms precancerous cells, the treatment is usually a minor procedure to remove them, often in the office. It's highly effective.
What's a colposcopy?
If your doctor recommends it, don't let the name scare you. It's essentially a close-up exam of your cervix. They use a special magnifying instrument (a colposcope) that stays outside your body. They might apply a vinegar solution to the cervix, which highlights any abnormal areas. If they see a suspicious spot, they'll take a tiny tissue sample (a biopsy). The biopsy pinches or cramps for a moment, but it's very quick. It's the definitive way to know what's going on.
How Often Do You Really Need a Pap Smear Test?
The guidelines have changed over the years, which causes confusion. The old "yearly Pap" is mostly gone. Current guidelines are based on age and history, and they aim to screen enough to catch problems but not so much that it leads to unnecessary procedures.
Here's a general breakdown, but always follow your own doctor's advice based on your personal health history:
- Under 21: Usually not recommended, regardless of sexual activity.
- 21-29: A Pap test alone every 3 years.
- 30-65: You have options: A Pap test alone every 3 years, OR an HPV test alone every 5 years, OR a Pap and HPV test together ("co-testing") every 5 years. This is the big change—the shift to less frequent screening when combined with HPV testing.
- Over 65: You may be able to stop screening if you've had adequate prior normal screenings and aren't at high risk.
These are for people with a cervix who are at average risk. You may need more frequent Pap smear tests if you have a history of abnormal results, are HIV-positive, have a weakened immune system, or were exposed to DES before birth.
Busting the Biggest Pap Smear Myths
Myth 1: "If I'm not sexually active, I don't need one."
While HPV is sexually transmitted, the guidelines for screening start at age 21 for everyone with a cervix, regardless of sexual history. It's still an important baseline.
Myth 2: "It's going to be extremely painful."
For most, it's not. Discomfort, pressure, awkwardness? Yes. Excruciating pain? Not typical. If it is painful, communicate that—it's valuable information for your provider about your body.
Myth 3: "An abnormal result means I have cancer."
Let's say it again: NO. It is a screening test designed to find changes long before cancer develops. An abnormal Pap is a call for more information, not a diagnosis.
Myth 4: "I'm too old for this."
Cervical cancer risk continues as you age. The decision to stop screening after 65 is based on a history of negative tests, not just age alone. Talk to your doctor.
Answers to Questions You're Too Embarrassed to Ask
The Bottom Line: Your Health, Your Power
Look, I get it. It's not fun. It's awkward and can be anxiety-provoking. But after learning more and seeing its impact, I've come to view my Pap smear appointment differently. It's not something that's being done to me. It's something I'm actively doing for myself. It's a powerful, proactive step in taking charge of my long-term health.
It's a few minutes of discomfort for years of peace of mind. And if something is found, it's almost always at a stage where it can be managed simply. That's the real win.
So if you've been putting it off because you're nervous or unsure, I hope this guide helped demystify things. Talk to your doctor about any specific concerns. Schedule the appointment. Get it done. And then go treat yourself to a coffee or whatever makes you happy. You've earned it.
POST A COMMENT