Mastering Bladder Control: Your Ultimate Guide to Freedom & Confidence
Quick Guide Overview
- What's Really Going On Down There? The Bladder Control Basics
- First Steps: The Lifestyle Audit for Better Bladder Control
- The Muscle Builders: Truly Effective Bladder Control Exercises
- When to Call in the Professionals
- Answering the Questions You're Too Embarrassed to Ask
- Wrapping It Up: Your Path Forward
Let's be honest for a second. How many times has the simple fear of not making it to the bathroom on time dictated your day? Maybe you've turned down a long car ride, hesitated before that second cup of coffee, or found yourself scanning for exit signs during a meeting. That constant, low-level anxiety is exhausting. It chips away at your spontaneity and confidence.
I remember talking to a friend who's an avid hiker. She told me she started mapping trails not by scenic views, but by the availability of restrooms. That's when it hit me—this isn't just a minor inconvenience; it's a quality of life issue. The good news? You're not powerless. Gaining better bladder control isn't about magic pills or superhuman willpower. It's about understanding how your body works and giving it the right tools. This guide is that toolkit.

What's Really Going On Down There? The Bladder Control Basics
Before we jump into solutions, let's get on the same page about the mechanics. It's hard to fix something if you don't know how it's supposed to function, right?
Your bladder is a hollow muscular organ (the detrusor muscle, if you want the technical term) that relaxes to store urine and contracts to release it. The real gatekeeper is your urethral sphincter—a group of muscles that act like a tight seal. All of this sits on a "hammock" of muscles called the pelvic floor. When you decide to go, your brain sends a signal, the pelvic floor and sphincter relax, the bladder muscle squeezes, and out it goes. Simple in theory.
So where does bladder control go wrong? Usually, it's a breakdown in one part of this team:
- The Muscles Get Weak: This is the classic culprit. Pregnancy, childbirth, aging, chronic coughing, or heavy lifting can weaken the pelvic floor muscles. A weak floor means poor support for the bladder and a weaker sphincter seal. The result? Stress incontinence—leaking when you cough, laugh, sneeze, or jump.
- The Nerves Get Confused: Sometimes the messaging system goes haywire. The bladder muscle might contract suddenly and forcefully without your permission, creating an overwhelming, can't-wait urge. This is the hallmark of overactive bladder (OAB). Conditions like diabetes, neurological diseases, or even a past UTI can contribute to this.
- The Brain-Bladder Chat Gets Noisy: For some, the issue is habit. Over time, you might have trained yourself to go "just in case" so often that your bladder's capacity shrinks, and it starts sending "FULL!" signals when it's only half-full.
See, it's rarely one single thing. It's often a combination. And that's actually hopeful, because it means there are multiple avenues for improvement.
First Steps: The Lifestyle Audit for Better Bladder Control
You'd be surprised how much impact your daily habits have. I'm not talking about drastic overhauls, but smart tweaks. Before you dive into exercises or doctor visits, try this audit. It's low-cost, zero-risk, and can yield significant results.
1. When you drink and how much.
2. When you urinate and an estimate of how much (think: stream strength, time).
3. When you have an urge or a leak, and what you were doing (sneezing, hearing water, etc.).
It's tedious, I know. But the patterns it reveals are pure gold. You might discover your leaks happen only after your third coffee, or that you're actually not drinking enough.
What You Sip Matters
Hydration is non-negotiable. But drinking less to avoid leaks is a terrible strategy. Concentrated urine irritates the bladder lining, which can increase urgency. The goal is steady, moderate intake.
Now, about the usual suspects:
- Caffeine: It's a diuretic and a bladder irritant. A double whammy. If you're serious about improving bladder control, cutting back is your biggest lever. Try switching to half-caff or limiting yourself to one cup in the morning.
- Alcohol: Another diuretic that can also numb your sensation of fullness, leading to accidental overfilling and then sudden urgency.
- Artificial Sweeteners & Acidic Foods: For some people, aspartame (in many diet sodas) and very acidic foods like tomatoes, citrus, and vinegar can be irritants. It's not universal, but worth experimenting with if you're sensitive.
Here’s a quick-reference table to guide your fluid choices:
| Beverage/Food | Effect on Bladder | Smart Strategy |
|---|---|---|
| Water | Ideal. Neutral and non-irritating. | Sip steadily throughout the day. Aim for pale yellow urine. |
| Coffee/Black Tea | Diuretic & irritant. Major trigger for urgency. | Limit to 1-2 cups, preferably before noon. Try herbal tea after. |
| Soda (Regular/Diet) | Carbonation & acids can irritate. Diet versions have sweeteners. | Treat as an occasional drink, not your main hydration. |
| Alcohol | Diuretic. Can impair sensation. | Have with plenty of water. Note if certain types (wine, beer) are worse. |
| Spicy Foods | Can be a direct irritant for many people. | Observe your body's reaction. You might tolerate mild spices but not hot peppers. |
Weight and Constipation: The Silent Contributors
This one is rarely talked about but so important. Excess weight, especially around the abdomen, puts constant downward pressure on your pelvic floor. Losing even 5-10% of your body weight can reduce leakage episodes dramatically. It's not about being skinny; it's about reducing the mechanical load on those muscles.
And constipation? A full rectum presses right against the bladder, reducing its capacity and irritating it. Straining during bowel movements also weakens the pelvic floor. A high-fiber diet and good hydration are foundational for both bowel and bladder control.
The Muscle Builders: Truly Effective Bladder Control Exercises
Alright, let's talk about the famous Kegels. Everyone says "do them," but almost nobody explains how to do them correctly. Doing them wrong is not just useless—it can make things worse by straining other muscles.
Finding Your Pelvic Floor (This is the Crucial First Step)
Try this: Next time you're urinating, try to slow or stop the stream mid-flow. Only do this once as a test! The muscles you use are your pelvic floor muscles. Remember that sensation. Now, the key is to isolate only those muscles. You shouldn't be squeezing your buttocks, thighs, or holding your breath. Place a hand on your lower belly—it should stay soft.
If you're struggling, don't panic. For some, especially after childbirth or with significant weakness, the connection is lost. A pelvic floor physical therapist is a game-changer here. They use biofeedback to help you see and activate the right muscles. The American Physical Therapy Association has a great tool to find a specialist near you.
The Right Way to Kegel
Once you've found them, here's the regimen:
- The Quick Flicks: Squeeze hard and fast, then release completely. Do 10-15 of these. This builds fast-twitch fibers for that reflexive squeeze when you cough or sneeze.
- The Long Holds: Squeeze and hold for 5-10 seconds (work up to it), then relax for twice as long (10-20 seconds). Aim for 10 reps. This builds endurance.
Do this set 3-4 times a day. The beauty is you can do them anywhere—at your desk, in traffic, watching TV. Consistency is everything. It takes 6-12 weeks to see real improvement, so be patient.
- Bearing Down: If you feel a pushing-out sensation, you're doing it backwards. Focus on a lifting and squeezing-in sensation.
- Forgetting to Relax: The release is as important as the squeeze. A constantly tense pelvic floor can cause pain and urgency.
- Holding Your Breath: Breathe normally! This ensures you're not using your abdominal muscles.
Beyond Kegels: Bladder Training
If urgency and frequency are your main issues, Kegels alone might not be enough. You need to retrain your bladder's schedule. This is called bladder training or timed voiding.
Using your bladder diary, find your current average time between bathroom trips. Let's say it's every hour. For the next week, make yourself wait an extra 15 minutes, even if you feel the urge. When the urge hits, don't sprint. Sit still, take slow deep breaths, and do a few strong pelvic floor contractions (the quick flicks) to inhibit the bladder muscle's spasm. Distract yourself. The urge will often pass. After a week of success, add another 15 minutes. The goal is to stretch intervals to a comfortable 3-4 hours.
It requires discipline, but it's incredibly effective for resetting an overactive bladder. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) has detailed patient guides on bladder control problems and training techniques that are worth a look.
When to Call in the Professionals
Look, if lifestyle changes and consistent exercises for 3 months aren't making a dent, it's time to see a doctor. This isn't failure; it's smart escalation. Persistent issues could signal something else that needs attention, like a recurrent infection, interstitial cystitis, or an anatomical issue.
A urologist or a urogynecologist (a gynecologist who specializes in pelvic floor disorders) can run tests like a urinalysis, a bladder scan to see if you're emptying completely, or even a urodynamic study to measure pressures. They can also discuss medical options.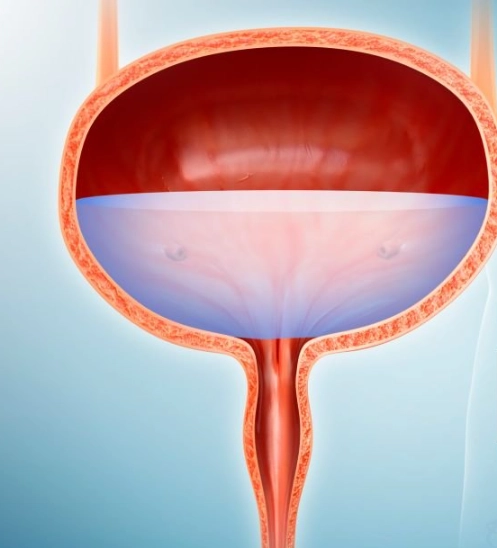
A Quick Rundown of Medical Options
I'm not a doctor, but here's what my research and conversations with specialists have shown me. Medications (like anticholinergics or beta-3 agonists) can calm an overactive bladder muscle. They have side effects for some people (dry mouth, constipation), so it's a trade-off to discuss.
For stress incontinence, a minor procedure like a urethral sling can provide mechanical support. It's very effective for the right candidate. There are also office-based treatments like Bulkamid or Pessaries. The point is, you have options beyond just "living with it." The American Urological Association provides excellent, peer-reviewed clinical guidelines for incontinence treatment that your doctor likely follows.
Answering the Questions You're Too Embarrassed to Ask
Wrapping It Up: Your Path Forward
The journey to reliable bladder control is a marathon, not a sprint. It requires patience and a bit of self-compassion. You didn't develop this issue overnight, and you won't fix it overnight either.
Start with the audit. Get curious about your own patterns. Then, commit to learning the proper exercises. If you hit a wall, seek out a professional—a physical therapist first, then a doctor if needed. This isn't a solitary struggle. There are resources and people who can help.
So take a deep breath. Pick one thing from this guide to try this week. Maybe it's starting that bladder diary. Maybe it's practicing finding those pelvic floor muscles. Just start. Your future, more confident self will thank you for it.
POST A COMMENT