Ovary Diseases List: Symptoms, Diagnosis & Treatment Guide
Let's talk about your ovaries. They're not just about reproduction; they're hormone powerhouses central to your overall health. When something goes wrong, the signs can be vague, confusing, and often brushed aside. You might search for an "ovary diseases list" because you're feeling off—maybe your periods have become unpredictable, or you have a lingering ache in your pelvis. You're looking for clarity.
This isn't just a dry list of medical terms. We're going to walk through the most common ovarian disorders, what they actually feel like, how doctors figure them out, and what you can do about it. I've seen too many women waste years thinking their symptoms are just "normal" discomfort or stress. Knowing what's on that list is the first step to taking control.
What You'll Find in This Guide
Common Ovary Diseases: A Detailed List
Here are the key conditions that make up a practical ovary diseases list. Think of them in categories: hormonal/functional issues, growths (cysts and tumors), and tissue-related problems.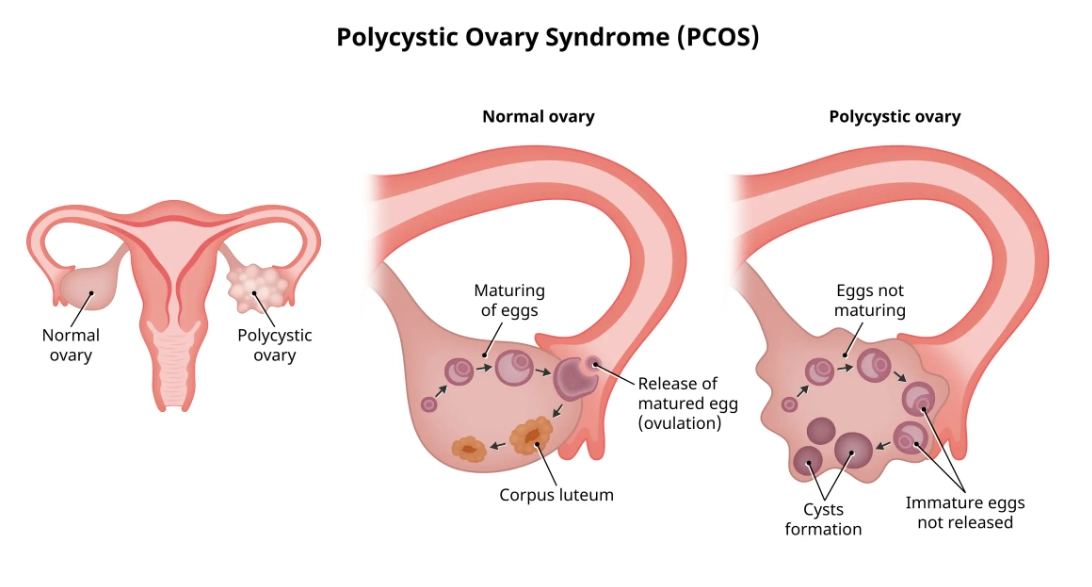
1. Polycystic Ovary Syndrome (PCOS)
The most common hormonal disorder in women of reproductive age. It's a metabolic and endocrine syndrome. The name is misleading—you don't necessarily have multiple "cysts," but many small, immature follicles that give the ovary a characteristic appearance on ultrasound. The root issue is often insulin resistance, which drives excess androgen (male hormone) production. The Centers for Disease Control and Prevention (CDC) estimates it affects 6-12% of women.
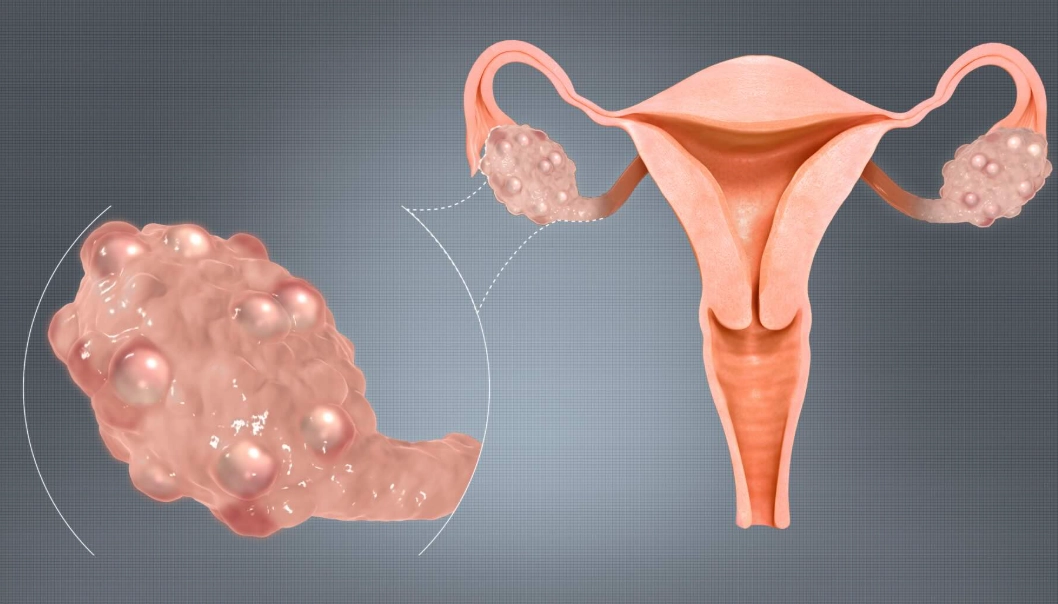
2. Ovarian Cysts
Fluid-filled sacs on or within an ovary. The vast majority are functional cysts (follicular or corpus luteum cysts), part of a normal menstrual cycle that just didn't dissolve. They're usually harmless and go away on their own. Then there are pathological cysts, like dermoid cysts (which can contain hair, teeth), cystadenomas, and endometriomas (related to endometriosis).
3. Endometriosis
This is when tissue similar to the uterine lining grows outside the uterus, often on the ovaries, forming "chocolate cysts" (endometriomas). It's a chronic inflammatory condition. The pain isn't from the cyst itself bursting, but from the inflammatory process and scarring. It's a major cause of pelvic pain and infertility.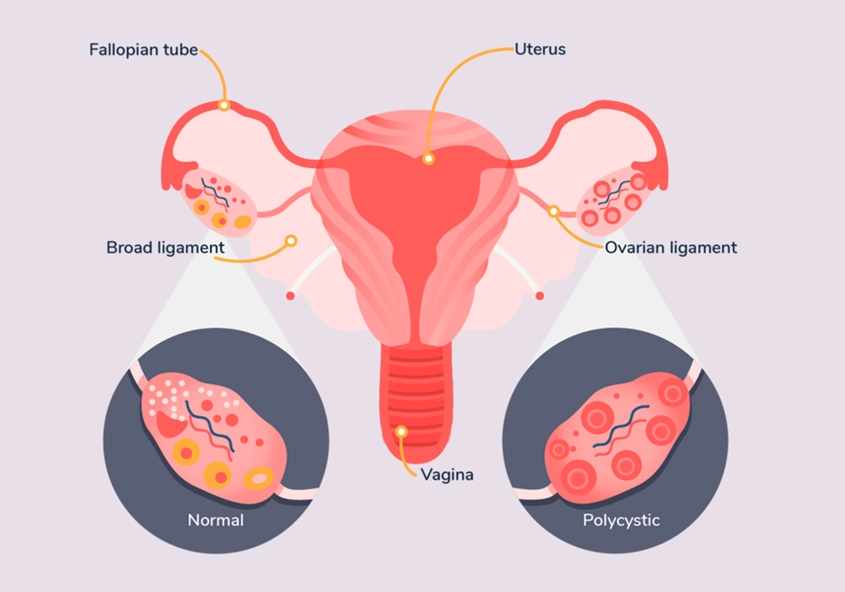
4. Primary Ovarian Insufficiency (POI)
Formerly called premature ovarian failure. This is when the ovaries stop working normally before age 40. It's not the same as menopause. Periods become irregular and then stop, estrogen levels drop. Causes can be genetic, autoimmune, or unknown. The emotional and physical impact—infertility, menopausal symptoms at a young age—is significant and often poorly addressed.
5. Ovarian Tumors (Benign and Malignant)
Growths that can be non-cancerous (benign) or cancerous (malignant).
- Benign: Examples include fibromas, Brenner tumors. They can cause pressure or pain but aren't life-threatening.
- Ovarian Cancer: A serious concern, often called a "silent killer" because symptoms are subtle until later stages. Major types include epithelial carcinoma (most common), germ cell tumors, and stromal tumors. According to the American Cancer Society, the lifetime risk is about 1 in 78.
6. Ovarian Torsion
A surgical emergency. This is when an ovary (often with a cyst) twists around its supporting ligaments, cutting off its blood supply. The pain is sudden, severe, and one-sided. It requires immediate medical attention to save the ovary.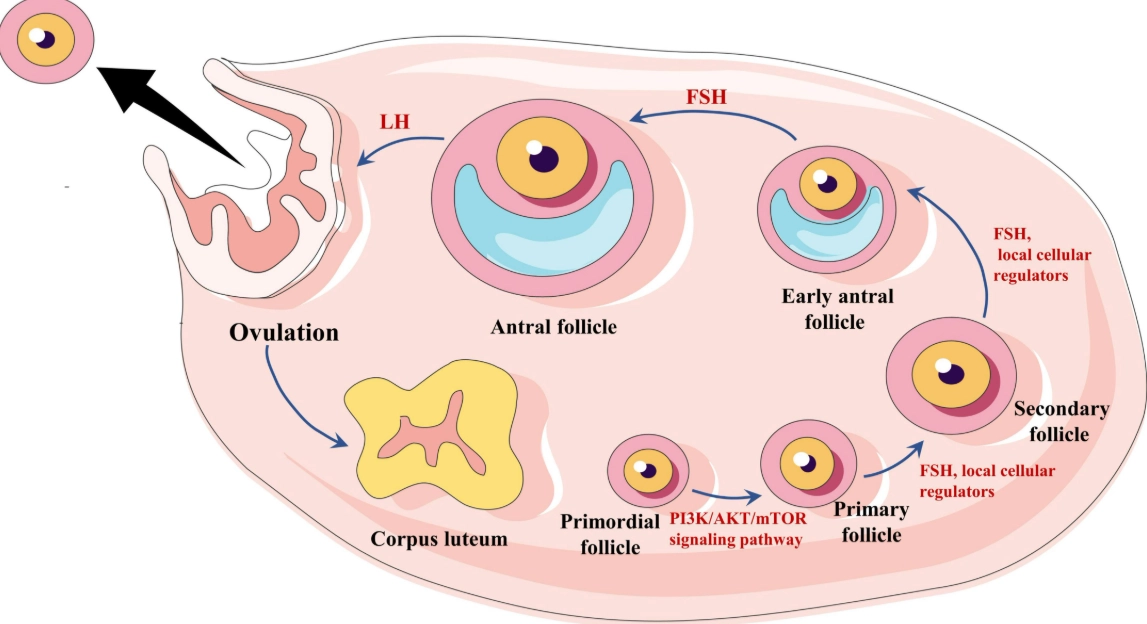
Symptom Breakdown: What Your Body is Telling You
Symptoms overlap, which is why diagnosis can be tricky. Here’s a clearer look at what to watch for.
| Symptom | Common in These Conditions | Important Notes |
|---|---|---|
| Pelvic Pain/Ache | Cysts, Endometriosis, Torsion, Cancer (later stage) | A constant dull ache differs from a sudden, stabbing pain (torsion or rupture). Endometriosis pain often correlates with your cycle. |
| Irregular Periods | PCOS, POI, Thyroid disorders | This is a huge red flag. Cycles shorter than 21 days, longer than 35 days, or wildly unpredictable need investigation. |
| Bloating & Feeling Full Quickly | Ovarian Cancer, Large Cysts | Persistent bloating that doesn't come and go with your cycle is a key symptom highlighted by organizations like the Mayo Clinic for ovarian cancer. |
| Excess Hair Growth & Acne | PCOS | Caused by high androgens. Look for hair on the face, chest, lower abdomen. |
| Pain During Sex | Endometriosis, Cysts, PID | Deep pain during or after intercourse is a classic sign of endometriosis. |
| Urinary Urgency/Frequency | Large Cysts, Tumors pressing on bladder | If it's not a UTI, consider pelvic pressure from a mass. |
How Are Ovarian Diseases Diagnosed?
It's not one test. It's a puzzle. Doctors start with a detailed history—your cycle history is gold. Then comes the physical exam, including a pelvic exam to check for tenderness or masses.
Transvaginal Ultrasound is the cornerstone imaging test. It gives a clear picture of the ovaries' size, shape, and internal structure. Is it a simple, fluid-filled cyst? A complex mass with solid areas? This guides the next steps.
Blood Tests look at different things:
- Hormone panels: FSH, LH, estrogen, testosterone, AMH. Crucial for diagnosing PCOS or POI.
- CA-125: A tumor marker. Here's the expert nuance: CA-125 is not a screening test for the general population. It can be elevated in endometriosis, fibroids, even normal menstruation. It's most useful for monitoring known ovarian cancer or assessing a post-menopausal woman with a complex pelvic mass.
Sometimes, advanced imaging like an MRI is needed. For a definitive diagnosis of cancer or severe endometriosis, a laparoscopy (keyhole surgery) allows direct visualization and biopsy.
Treatment Paths and Management Strategies
Treatment is as varied as the conditions themselves. It targets symptoms, preserves fertility if desired, and manages long-term risks.
For Hormonal Disorders (PCOS, POI)
Lifestyle change is first-line therapy for PCOS, not an afterthought. A 5-10% weight loss can restart ovulation and improve insulin sensitivity. Metformin is often used for insulin resistance. Hormonal birth control regulates cycles and manages acne/hair growth. For POI, hormone replacement therapy (HRT) is critical for bone and heart health.
For Cysts and Growths
Watchful Waiting: For simple cysts under 5cm in premenopausal women, repeat ultrasound in a few months.
Surgery: Considered for large cysts (>5-10cm), complex/suspicious cysts, persistent painful cysts, or suspected torsion. Options range from cystectomy (removing just the cyst) to oophorectomy (removing the ovary).
For Endometriosis
Pain meds, hormonal therapies (like progestins or GnRH agonists) to suppress menstruation, and laparoscopic surgery to excise or ablate endometrial implants. There's no cure, so management is chronic.
For Ovarian Cancer
Treatment typically involves a combination of surgery (often a total hysterectomy with removal of both ovaries and fallopian tubes) and chemotherapy. Genetic testing for BRCA mutations is now standard, as it affects treatment choices and screening for family members.
The one thing I stress to everyone: you must be your own advocate. If your symptoms are dismissed and you know something's wrong, seek a second opinion. Find a gynecologist who listens, or see a reproductive endocrinologist for complex issues like PCOS or POI.
POST A COMMENT