Ovarian Disorders Guide: Symptoms, Treatments & Daily Management
Sarah thought the sharp pain on her right side was just a bad cramp. It came and went for weeks. When an ultrasound finally revealed a 4cm ovarian cyst, her doctor tossed out phrases like "probably benign" and "watchful waiting." The uncertainty was worse than the pain. Her story isn't unique. Ovarian disorders, from common cysts to complex syndromes like PCOS, create a fog of confusion for millions. They're often shrouded in vague symptoms and generic advice that leaves you managing fear as much as the condition itself.
Let's cut through that fog. This isn't a medical textbook rehash. It's a practical map built from conversations with specialists and the lived experiences of women navigating these diagnoses. We'll move beyond basic definitions into the nuances that actually affect your life—like when a cyst size truly matters, why PCOS treatment fails if you only focus on the pill, and the subtle signs of premature ovarian failure that most people miss.
In This Article
- Understanding the Spectrum of Ovarian Disorders
- Ovarian Cysts: A Deep Dive Beyond the Basics
- PCOS: Moving Past Birth Control to Comprehensive Management
- Premature Ovarian Failure: The Early Menopause Puzzle
- The Diagnosis and Treatment Path: What to Really Expect
- Daily Life Strategies: Management Beyond Medication
Understanding the Spectrum of Ovarian Disorders
Your ovaries aren't just egg warehouses. They're endocrine powerhouses, central to your fertility, cycle, and overall hormonal harmony. When they malfunction, the effects ripple out. The term "ovarian disorders" covers a lot of ground, but three conditions account for the vast majority of concerns and doctor visits.
Ovarian Cysts: Fluid-filled sacs that are incredibly common. Most are functional—tied to your menstrual cycle—and vanish on their own. The anxiety starts when they don't, or when they cause pain.
Polycystic Ovary Syndrome (PCOS): This is a metabolic and endocrine disorder masquerading as a reproductive one. The name is misleading; it's not really about the cysts. It's a syndrome characterized by hormonal imbalance (high androgens), irregular ovulation, and often, insulin resistance. According to the American College of Obstetricians and Gynecologists (ACOG), it affects about 1 in 10 women of childbearing age.
Premature Ovarian Failure (POF) / Primary Ovarian Insufficiency (POI): This is when the ovaries call it quits before age 40. Egg supply dwindles, estrogen production drops, and periods become sporadic or stop. It's less common but carries significant long-term health implications for bone and heart health.
The biggest mistake? Treating them all the same. A cyst and PCOS require completely different management mindsets.
Ovarian Cysts: A Deep Dive Beyond the Basics
You get an ultrasound report that says "left ovarian cyst, 3cm." Panic sets in. Let's demystify this.
Most cysts are functional. A follicular cyst forms if the follicle doesn't release its egg. A corpus luteum cyst forms after ovulation if the sac reseals and fills with fluid. These are signs of your ovary doing its job, albeit clumsily. They usually resolve in one to three cycles.
Then there are pathological cysts, like dermoids or cystadenomas. These aren't tied to the cycle and won't go away on their own. They're often the ones that grow large or have weird stuff inside (like hair or teeth, in the case of dermoids).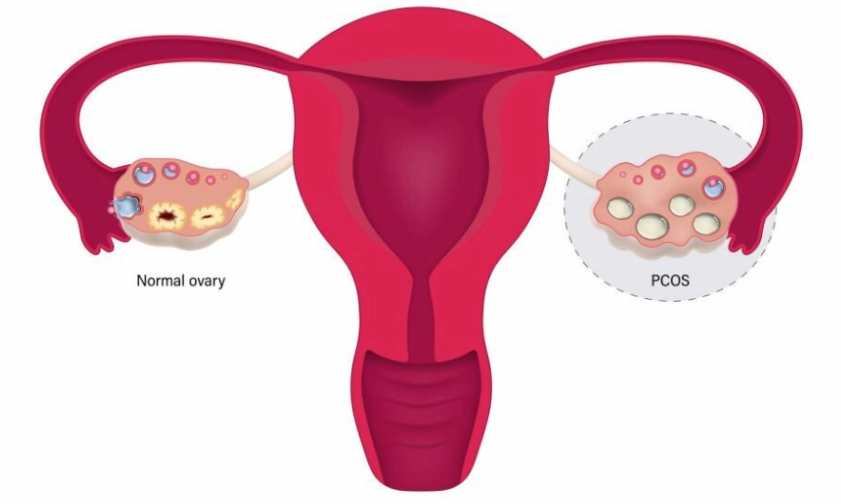
When Should You Actually Worry About a Cyst?
Doctors throw around the "5cm rule," but it's a guideline, not a law. I've seen 7cm simple cysts be monitored safely and 3cm complex ones warrant surgery. The decision matrix looks at more than size:
- Ultrasound Appearance: Is it simple (fluid-filled, thin wall) or complex (with solid areas, internal walls, or debris)? Complex features raise a flag.
- Symptoms: Persistent, severe pain, especially if sudden (hinting at torsion or rupture), bloating, or pressure on your bladder.
- Your Age: New cysts in postmenopausal women are taken more seriously due to a statistically higher, though still small, risk of malignancy.
- Growth: A cyst that grows steadily over 2-3 follow-up scans is a candidate for removal.
The standard protocol is "watchful waiting" with a repeat ultrasound in 6-12 weeks. It's frustrating, but it's often the medically sound approach. Jumping to surgery for an asymptomatic simple cyst is usually overkill and introduces its own risks.
PCOS: Moving Past Birth Control to Comprehensive Management
If I had a dollar for every woman told to "just take the pill" for PCOS and sent on her way, I'd be rich. It's the classic band-aid. The pill regulates bleeds and can clear acne, but it does nothing for the root cause for many: insulin resistance.
Think of insulin resistance as your cells becoming deaf to insulin's knock. Your pancreas pumps out more, and this high insulin level tells your ovaries to overproduce testosterone. This leads to the classic PCOS triad: irregular periods, excess hair growth/acne, and those tell-tale "cysts" (which are actually immature follicles) on ultrasound.
The PCOS Management Pillar Most People Skip: Lifestyle intervention isn't just nice advice; it's first-line therapy. Research cited by the American Society for Reproductive Medicine shows that losing just 5-10% of your body weight can restart ovulation and improve metabolic markers. But it's not about crash dieting. A low-glycemic index diet—swapping white bread and sugar for whole grains, protein, and healthy fats—directly lowers insulin demand. Pair this with regular exercise (both cardio and strength training), and you're treating the engine, not just the dashboard lights.
Beyond the pill and lifestyle, medications like metformin improve insulin sensitivity directly. For fertility, drugs like letrozole are often more effective than clomiphene for inducing ovulation in PCOS. The point is, your treatment plan should be layered. If your doctor only offers birth control, it's worth seeking a second opinion from an endocrinologist or a reproductive endocrinologist.
Premature Ovarian Failure: The Early Menopause Puzzle
POF/POI is a tough diagnosis. It often feels like your body's clock has shattered. The signs are sneaky: periods becoming light and infrequent, hot flashes at 35, a nosedive in libido, or a creeping sense of brain fog and irritability that you blame on stress.
Diagnosis hinges on blood tests taken twice, about a month apart:
Follicle-Stimulating Hormone (FSH): Levels over 25-30 mIU/mL are indicative.
Anti-Müllerian Hormone (AMH): This measures your ovarian reserve. A very low AMH aligns with POF.
Estradiol: Often low.
It's a grief process—for fertility, for your sense of a predictable future. But it's not the end of your health. The critical follow-up is addressing the estrogen deficit. Without estrogen, bone loss accelerates and heart disease risk increases. Hormone replacement therapy (HRT) until the natural age of menopause (around 51) is typically recommended to protect your bones, heart, and brain, and to manage those menopausal symptoms. This is a crucial conversation to have with your doctor.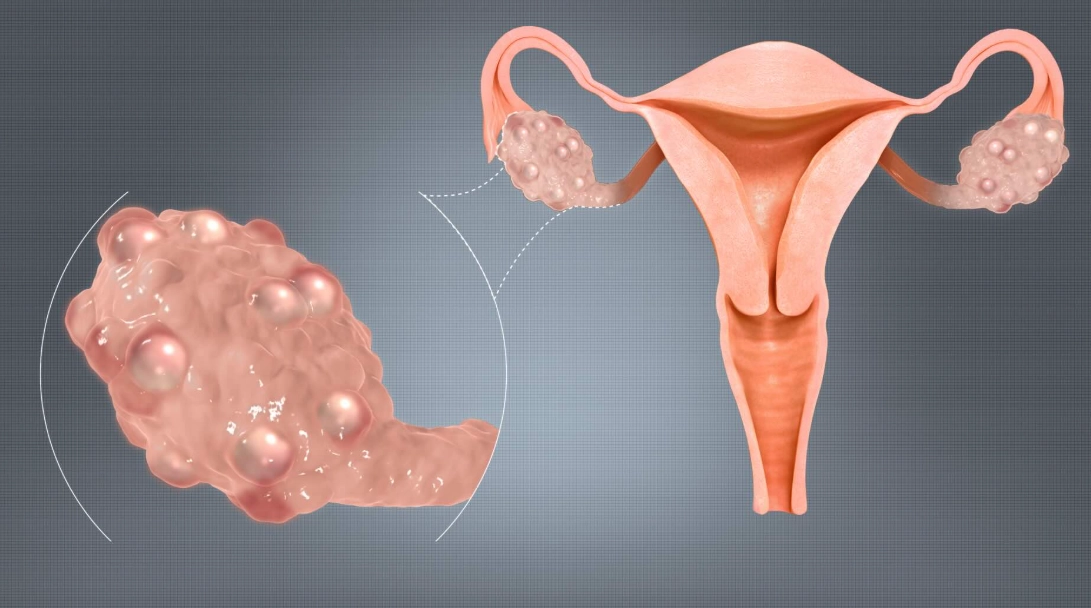
The Diagnosis and Treatment Path: What to Really Expect
Navigating the medical system for an ovarian issue can feel like wandering a maze. Here's the typical roadmap, so you know what's coming.
Step 1: The Initial Workup. It starts with a detailed history and a pelvic exam. Then comes the ultrasound—the transvaginal one gives the clearest picture of your ovaries. They'll measure the cyst(s), describe its contents, and check blood flow.
Step 2: The Blood Tests. This isn't random. They're looking for:
- CA-125: A tumor marker. Important context: It's notoriously non-specific. It can be elevated in endometriosis, fibroids, or even during your period. A high CA-125 with a complex ovarian mass is concerning; a slightly elevated one with a simple cyst is far less so.
- Hormone panels (FSH, LH, testosterone, AMH): Crucial for diagnosing PCOS or POF.
- Pregnancy test: Always rule this out first.
Step 3: The Decision Point. Your doctor will synthesize the ultrasound details, your symptoms, age, and blood work. The options are:
Monitor: The most common path for simple cysts.
Medicate: Like birth control for PCOS/cyst prevention, or HRT for POF.
Operate (Laparoscopy or Laparotomy): For large, persistent, complex, or symptomatic cysts, or for cyst removal to confirm diagnosis (like with a dermoid).
Daily Life Strategies: Management Beyond Medication
Living well with an ovarian disorder means building a supportive lifestyle. Medication handles the acute issues, but your daily habits build resilience.
Diet Tweaks That Actually Help:
- For PCOS/Cysts: Focus on anti-inflammatory foods. Reduce sugar and refined carbs to manage insulin. Increase fiber, lean protein, and loads of colorful vegetables. Some find dairy inflammatory; it's worth a 3-week trial elimination to see if symptoms improve.
- For POF/General Support: Prioritize calcium and vitamin D for bone health (think leafy greens, fortified foods, safe sun exposure). Healthy fats (avocado, nuts, olive oil) support hormone production.
Movement Matters: Regular exercise reduces insulin resistance (key for PCOS), manages stress (which can worsen all hormonal issues), and strengthens bones. You don't need to run marathons. Consistency with brisk walking, yoga, or strength training is what counts.
Stress is a Hormone Disruptor: Chronic stress raises cortisol, which can throw other hormones like estrogen and progesterone out of whack. This isn't woo-woo; it's endocrinology. Find your pressure valve—meditation, journaling, time in nature, saying "no" more often.
Track Your Cycle: Even if it's irregular. Apps or a simple journal noting energy, mood, pain, and bleeding patterns can reveal triggers and help you communicate more effectively with your doctor.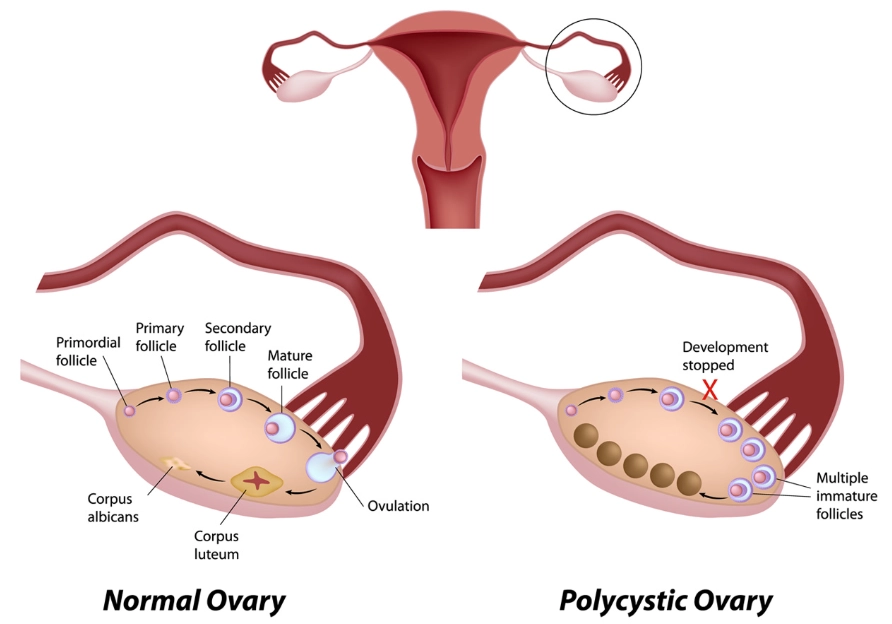
The journey with an ovarian disorder is marathon, not a sprint. It's filled with waiting rooms, unclear scans, and trial-and-error with treatments. Arm yourself with specific questions for your doctor, advocate for comprehensive testing, and remember that managing your overall metabolic and mental health is just as important as treating the ovary itself. Knowledge, paired with a proactive care team, is your most powerful tool.
POST A COMMENT