Understanding and Managing Incontinence in Women: A Complete Guide
Quick Guide
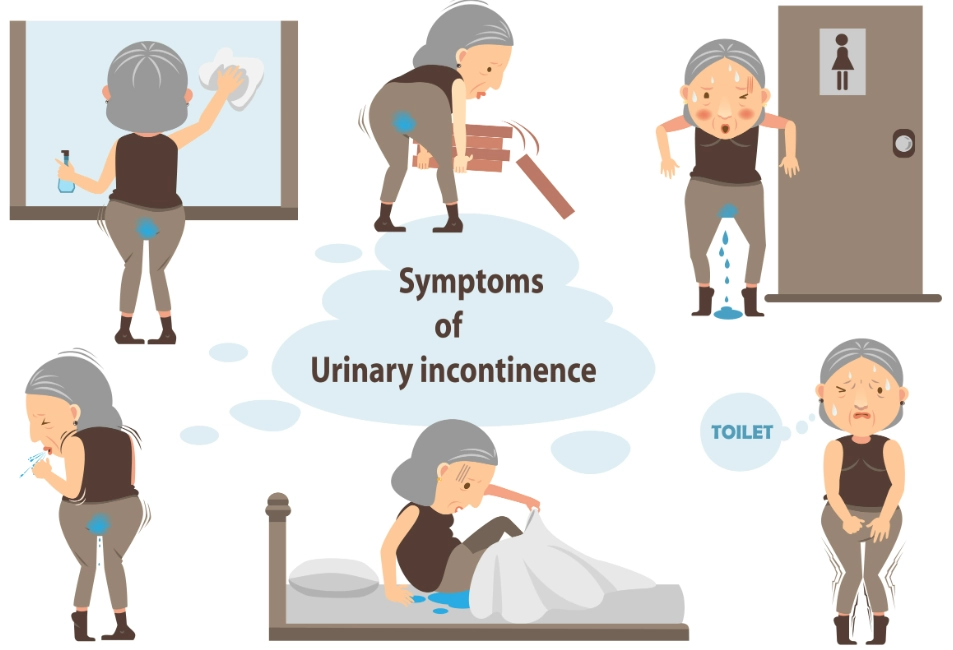
Let's talk about something that affects millions but often gets whispered about in shame. Incontinence in women. It's that unexpected leak when you laugh too hard, cough, or even just stand up. You might think you're alone, but believe me, you're not. So many women deal with this, and the first step to taking back control is understanding what's really going on.
I remember a friend confiding in me years ago. She loved running but had started avoiding her morning jog because of little accidents. She thought it was just her, a personal failing. It took her ages to even mention it to her doctor. That's the stigma talking. The truth is, female urinary incontinence is a medical condition, not a character flaw. It's a signal from your body, and it's one we can learn to manage.
What Exactly Is Incontinence in Women?
At its core, it's the involuntary loss of urine. Simple as that. But the reasons behind it? That's where it gets more complex. Your bladder, urethra, pelvic floor muscles, and nerves all have to work in perfect harmony. When that system is disrupted, leaks can happen.
It's not just about getting older. Sure, age can be a factor, but I've heard from women in their 20s and 30s struggling with this, especially after having kids. Blaming it purely on aging is a myth that stops people from seeking help. There are specific, treatable reasons for bladder control problems in women.
The Main Types of Female Urinary Incontinence
Not all leaks are the same. Knowing which type you're dealing with is half the battle. Doctors typically categorize them into a few main groups.
Stress Incontinence
This is the classic "laugh-pee" or "cough-pee." It happens when physical pressure (stress) on your bladder overwhelms your urethra's ability to stay closed. The trigger is a sudden increase in abdominal pressure.
- Common Causes: Childbirth (especially vaginal delivery), menopause (due to dropping estrogen levels), obesity, high-impact exercise, chronic coughing.
- What it feels like: A small, quick leak coinciding with the physical action. You don't usually feel a strong urge to go first.
Urge Incontinence (Overactive Bladder - OAB)
This one is all about a sudden, intense, and often uncontrollable need to urinate. Your bladder muscle (the detrusor) contracts involuntarily, giving you very little warning.
- Common Causes: Can be idiopathic (no clear cause), neurological conditions (like MS, stroke, Parkinson's), bladder irritation (from infections, stones), or simply aging changes.
- What it feels like: A powerful, gotta-go-NOW sensation that often leads to leaking before you can reach the toilet.
Mixed Incontinence
This is, unfortunately, very common. It's a combination of both stress and urge symptoms. You might leak when you sneeze and also have those urgent dashes to the bathroom. Treating mixed incontinence often requires a multi-pronged approach.
Overflow Incontinence
Less common in women than men, but it happens. This is when the bladder doesn't empty properly and becomes overfull, leading to constant dribbling or frequent leaks of small amounts. It can feel like you're never fully empty.
See? Just knowing the types helps make sense of the experience. It's not random.
Root Causes and Risk Factors for Bladder Control Problems
It's rarely one single thing. It's usually a combination. Let's break down the big contributors.
Pregnancy and Childbirth: This is a huge one. Carrying a baby puts prolonged pressure on the pelvic floor. Vaginal delivery can stretch and sometimes damage the muscles and nerves that control the bladder and urethra. The more vaginal births, the higher the risk, generally. But let's be clear—it's not a guarantee. Many women have multiple kids with no issues, while others have one child and struggle. Genetics and other factors play a role.
Menopause and Hormones: Estrogen helps keep the tissues of the urethra and vagina healthy, thick, and elastic. When estrogen levels drop during menopause, these tissues can thin out (a condition called urogenital atrophy) and become weaker. This can directly contribute to stress incontinence and can also cause urinary urgency.
Lifestyle Factors You Can Actually Change:
- Obesity: Extra weight increases constant pressure on the bladder and pelvic floor. The good news? Even a modest weight loss of 5-10% can significantly improve symptoms. It's one of the most effective non-surgical treatments.
- Smoking: The chronic cough associated with smoking is a major aggravator for stress incontinence. Plus, nicotine is a bladder irritant for some people.
- Diet: Caffeine and alcohol are diuretics (they make you produce more urine) and bladder irritants. Carbonated drinks, artificial sweeteners (like aspartame and saccharin), spicy foods, and very acidic foods (citrus, tomatoes) can be triggers for people with sensitive bladders.
- Constipation: Chronic straining puts immense pressure on the pelvic floor muscles, stretching and weakening them over time.
Other Medical Conditions: Diabetes (can cause nerve damage and increased urine output), neurological diseases, recurrent UTIs, and previous pelvic surgeries (like a hysterectomy) can all be factors.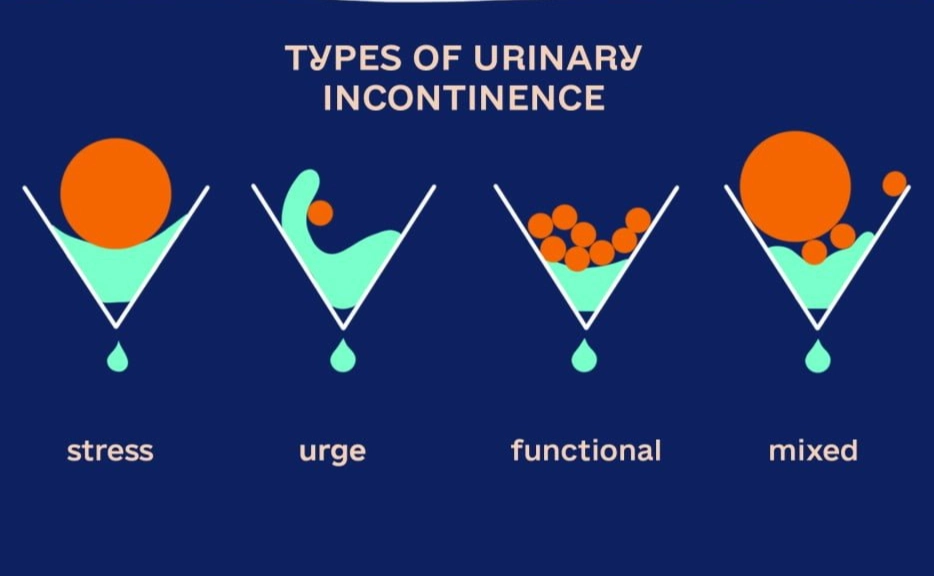
Taking Control: Management and Treatment Strategies
Okay, so we know the what and the why. Now for the good part—the what now. The goal isn't always a 100% cure (though that's possible for some), but rather significant improvement and regaining your confidence and freedom. Treatment is almost always a step-by-step ladder, starting with the least invasive options.
First-Line Defense: Lifestyle and Behavioral Modifications
Don't skip this part thinking it's too simple. For many women, these changes make a world of difference.
Bladder Training: This is for urge incontinence. You gradually increase the time between bathroom trips. Start by delaying urination by 15 minutes when you feel the urge. Over weeks, try to extend that to 2-4 hours. It's retraining your bladder's overactive signals.
Fluid Management: This doesn't mean drinking less! Dehydration concentrates your urine, which can irritate the bladder. Aim for about 6-8 glasses of fluid spread evenly through the day. Cut back 2-3 hours before bed to reduce nighttime trips. The key is the right amount, timed well.
Dietary Tweaks: Try eliminating common irritants (coffee, tea, soda, alcohol, artificial sweeteners) for two weeks. Then reintroduce them one at a time to see if any are your personal trigger. You might be surprised.
Weight Management: I know, easier said than done. But even a little bit helps. One study published by the National Institutes of Health (NIH) showed that a 5-10% weight loss led to a 50-60% reduction in incontinence episodes for overweight women. That's a huge return on investment.
The Golden Standard: Pelvic Floor Muscle Training (Kegels)
Ah, Kegels. Everyone's heard of them, but almost nobody does them correctly. They are the single most effective conservative treatment for stress incontinence and a big help for mixed incontinence.
But you have to do them right. Clenching your buttocks or holding your breath is wrong. You need to isolate the muscles you use to stop the flow of urine mid-stream. Hold for a count of 5-10 seconds, relax for the same amount, and repeat. Aim for 3 sets of 10-15 per day.
Medical Devices and Aids
These aren't giving up; they're practical tools.
- Pessaries: A silicone device inserted into the vagina to support the bladder neck and urethra. Great for stress incontinence, especially if surgery isn't an option. A doctor fits you for the right size and shape.
- Urethral Inserts: A small, disposable tampon-like device placed in the urethra to block leakage, removed before urination. Useful for specific activities like sports.
- Absorbent Products: The technology here has come a long way. From discreet liners and pads to specially designed underwear (like Thinx or Knix), they provide security and peace of mind while you work on other treatments. Don't see them as a failure; see them as your safety net.
Medications
Mainly used for urge incontinence/OAB. They work by relaxing the bladder muscle to reduce involuntary contractions.
| Medication Type | How It Works | Common Side Effects to Watch For |
|---|---|---|
| Anticholinergics (e.g., Oxybutynin, Tolterodine) |
Blocks the nerve signals that cause bladder muscle spasms. | Dry mouth, constipation, blurred vision, dizziness. Can worsen cognitive function in older adults. |
| Beta-3 Agonists (e.g., Mirabegron) |
Relaxes the bladder muscle to allow it to hold more urine. | Increased blood pressure, headache, possible UTI risk. |
| Topical Vaginal Estrogen | Replenishes estrogen locally to strengthen urethral/vaginal tissues (great for post-menopausal women). | Minimal systemic absorption. Some vaginal spotting/irritation possible. |
Medications require a doctor's prescription and supervision. They often work best combined with behavioral changes.
Procedures and Surgeries
These are typically considered when conservative measures haven't provided enough relief, especially for stress or mixed incontinence.
Bulking Agents: A minimally invasive procedure where a gel-like substance is injected into the tissue around the urethra to add bulk and help it close better. It can be done in a doctor's office. Results may fade over time and require repeat injections.
Nerve Stimulation:
- Percutaneous Tibial Nerve Stimulation (PTNS): A fine needle electrode is placed near the ankle to stimulate the tibial nerve, which connects to the nerves controlling the bladder. Weekly 30-minute treatments for 12 weeks.
- Sacral Neuromodulation: A pacemaker-like device is implanted under the skin to send mild electrical pulses to the sacral nerves. It's more invasive but can be very effective for both urge and certain cases of urinary retention.
Sling Procedures: The most common surgery for stress incontinence. A sling (made of synthetic mesh or your own tissue) is placed under the urethra like a hammock to provide support when you cough or strain. It's highly effective. The mesh controversy in recent years was related to pelvic organ prolapse repairs, not stress incontinence slings, but it's crucial to have a detailed discussion with a specialist urologist or urogynecologist about risks and benefits. You can find excellent, balanced information from the American Urological Association (AUA) to prepare for that conversation.
Answering Your Burning Questions (FAQs)
Let's tackle some of the specific things women are searching for.

Dealing with incontinence in women can feel isolating, but it's a path well-traveled. The solutions exist. It starts with shifting your mindset from shame to problem-solving. See your body as giving you information. Then, take one small step. Maybe it's starting a bladder diary. Maybe it's booking that appointment you've been putting off. Maybe it's just buying a pack of those absorbent underwear to get your confidence back so you can go for that walk or laugh with friends without worry.
Progress, not perfection. That's the goal with managing bladder control problems. You can get a huge chunk of your life and peace of mind back. You really can.
POST A COMMENT