Colorectal Cancer in Women: A Comprehensive Guide to Symptoms, Risks & Prevention
Key Points in This Guide
- Why Should Women Pay Special Attention to Colorectal Cancer?
- Spotting the Signs: Symptoms of Colorectal Cancer in Women
- Understanding Your Risk: It's More Than Just Family History
- Screening: The Single Most Powerful Tool You Have
- If You Hear the Words "It's Cancer": Navigating Diagnosis and Treatment
- Life After Treatment: Survivorship and Follow-Up Care
- Prevention: What Can You Actually Do?
Let's talk about something that doesn't get enough airtime in women's health circles. We're all pretty good about scheduling our mammograms and pap smears, right? But how many of us give the same priority to our colon health? I know I didn't, not until a close friend in her forties was diagnosed. It was a wake-up call that made me dive deep into understanding colorectal cancer in women. What I found surprised me – the symptoms can be sneaky, the risks are specific, and the information out there can be confusing.
You might think it's an "old man's disease," but that's a dangerous misconception. The reality is that colorectal cancer doesn't discriminate by gender. In fact, for women, the journey from first symptom to diagnosis can be particularly fraught. Symptoms often get brushed off as something else – maybe IBS, maybe just stress, maybe a gynecological issue. That delay can cost precious time.
So, I've put together this guide. Think of it as a long chat with someone who's done the homework, sifted through the medical jargon, and talked to experts. We'll cover everything from the subtle early warnings your body might be sending to the practical steps you can take today to protect yourself. Whether you're here out of curiosity, concern for a loved one, or because something just doesn't feel right, you're in the right place.
Why Should Women Pay Special Attention to Colorectal Cancer?
It's a fair question. Cancer is cancer, so why single out women? Well, the biology and the social context create a unique picture. For starters, the anatomy. A woman's pelvis houses both the reproductive organs and the lower part of the colon and rectum. This closeness means that symptoms of colorectal cancer can easily be mistaken for common gynecological problems like ovarian cysts, endometriosis, or even just menstrual cramps. A tumor pressing in that area doesn't send a memo saying "I'm in your colon." The pain or pressure feels general.
Then there's the societal bit. Women are often socialized to be caretakers, to put their own health last. Reporting embarrassing symptoms like changes in bowel habits or rectal bleeding? That can feel uncomfortable, leading to delays in speaking up. I've heard from more than one woman who said they felt "silly" bringing it up, or hoped it would just go away.
And let's not forget the hormonal piece. Research is ongoing, but there appears to be a complex relationship between estrogen, hormone replacement therapy, and colorectal cancer risk. Some studies suggest that factors like age at first period, number of pregnancies, and menopausal status might play a role. It's not straightforward, which is why having a doctor who listens to your whole health history is crucial.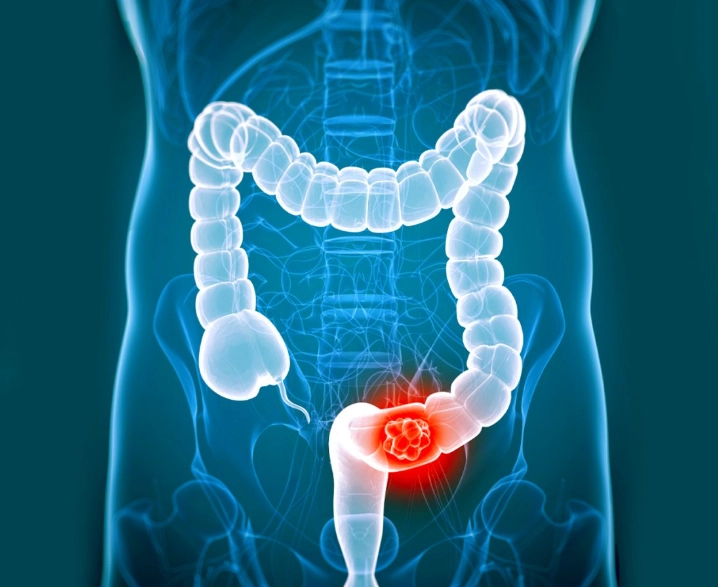
Spotting the Signs: Symptoms of Colorectal Cancer in Women
This is where things get tricky. The symptoms are often vague and nonspecific. They creep up slowly. You might adjust your life around them without even realizing it. Here’s a breakdown of what to watch for, beyond the obvious.
The Not-So-Obvious Symptoms
Everyone knows about rectal bleeding. But what about the subtler stuff?
- Unexplained Iron-Deficiency Anemia: This is a big one, especially for premenopausal women who might blame heavy periods. But if you're feeling constantly wiped out, look pale, get short of breath easily, and your iron is low despite a good diet or supplements, it's a red flag. The colon could be bleeding slowly, unnoticed.
- A Change in Bowel Habits That Just... Sticks: Not just a day or two of constipation. I'm talking about a persistent change that lasts for more than a few weeks – new constipation, diarrhea, or a feeling that your bowel doesn't empty completely. The consistency of your stool changing to pencil-thin can also be a sign of an obstruction.
- Persistent Abdominal Discomfort: Cramps, gas, pain, or a general feeling of fullness or bloating that doesn't resolve. The kind that makes you unbutton your pants after a meal, even a small one.
- Unexplained Weight Loss: Losing weight without trying is never normal. It's your body using extra energy to deal with something.
- Fatigue That Won't Quit: Not the "I had a busy week" tired. The deep, bone-weary fatigue that sleep doesn't fix. Often linked to anemia.
For women, pelvic pressure or pain can also be a symptom if the cancer is located low in the rectum. It's so easy to attribute this to gynecological causes. A friend's aunt spent a year seeing her gynecologist for pelvic pain before someone thought to check her colon.
Understanding Your Risk: It's More Than Just Family History
When we talk about risk for colorectal cancer in women, family history is the headline everyone knows. But it's only part of the story. Your daily choices and your personal medical history weigh heavily.
Let's break down the risk factors. I find a table helpful here to see the whole picture.
| Risk Factor Category | Specific Factors for Women | What You Can Do |
|---|---|---|
| Unchangeable Factors | Age (risk increases after 50, but rising in younger adults) Personal history of colorectal polyps or cancer Personal history of inflammatory bowel disease (Crohn's, UC) Family history of colorectal cancer or polyps |
Get screened on time. Know your family history and share it with your doctor. |
| Lifestyle Factors | Diet high in red/processed meats Low fiber intake Physical inactivity Obesity (fat tissue produces estrogen & inflammatory factors) Heavy alcohol use Smoking |
This is your area of control. Modifying these can significantly lower risk. |
| Medical & Hormonal Factors | Type 2 Diabetes Radiation therapy to the abdomen/pelvis (e.g., for prior cancers) Complex relationship with reproductive history & hormones (still being studied) |
Manage diabetes well. Discuss your full history with all your doctors. |
See that last row? The hormonal piece is fascinating. Some large studies, like those referenced by the National Cancer Institute, have suggested that postmenopausal hormone therapy (estrogen plus progestin) might be linked to a reduced risk of colorectal cancer. But – and this is a huge but – the same therapy increases the risk of breast cancer and other serious conditions. It's never a simple trade-off, and it's absolutely not a prevention strategy. This is why personalized medical advice is irreplaceable.
Screening: The Single Most Powerful Tool You Have
If I could get one message across, it's this: screening saves lives. It's not about finding cancer when you have symptoms. It's about finding precancerous polyps before they turn into cancer, or finding cancer at its earliest, most treatable stage. The difference in outcomes is staggering.
The guidelines have changed recently because of the alarming rise in cases among younger adults. It's not just an older person's concern anymore.
So, what are your options? There are several, each with pros and cons.
Colonoscopy: The Gold Standard
Yes, the prep is famously unpleasant. Let's not sugarcoat it. Drinking that gallon of liquid is no one's idea of a good time. But here's the thing – it's a one-day hassle for potentially years of peace of mind. A colonoscopy allows the doctor to visually inspect your entire colon and rectum and remove any polyps they find during the same procedure. That's prevention in action. The procedure itself is done under sedation, so you don't feel a thing. The American College of Gastroenterology provides excellent patient resources on what to expect, which can demystify the process. If you're at average risk and your colonoscopy is clear, you're typically good for another 10 years.
Stool-Based Tests
These are non-invasive and you can do them at home. They look for hidden blood (FIT test) or altered DNA (Cologuard) in your stool, which can be signs of cancer or large polyps.
- The Upside: No prep, no sedation, no time off work. Much easier to say yes to.
- The Catch: They are less accurate than a colonoscopy. They can miss some cancers and polyps, and they can give false-positive results (saying there's a problem when there isn't). Most importantly, if the test is positive, you will need a colonoscopy to follow up. They are not a replacement for colonoscopy; they are an alternative for people who refuse or cannot have a colonoscopy. They need to be done every 1-3 years depending on the test.
My personal take? If you can manage it, go for the colonoscopy. It's more thorough and gives you the longest interval. But if the thought of a colonoscopy fills you with dread and makes you put off screening entirely, then a stool test is infinitely better than doing nothing. The best test is the one you'll actually do.
If You Hear the Words "It's Cancer": Navigating Diagnosis and Treatment
This is the part no one wants to think about. But knowledge is power, and understanding the process can make it feel less terrifying. A diagnosis of colorectal cancer in women follows a clear path.
First, there's the diagnosis itself, usually confirmed by a biopsy during a colonoscopy. Then comes staging – figuring out how advanced the cancer is. This involves scans like CT scans, MRIs (especially for rectal cancer), and sometimes PET scans. The stage (0 through IV) determines the treatment plan.
Surgery has come a long way. Minimally invasive laparoscopic or robotic-assisted surgery means smaller incisions, less pain, and faster recovery for many patients. For rectal cancer, surgical techniques can often preserve the sphincter muscles, avoiding a permanent colostomy.
One significant aspect for women is fertility. Chemotherapy and radiation can affect ovarian function. If you are of childbearing age and wish to have children in the future, discussing fertility preservation options (like egg freezing) with your oncologist before starting treatment is critical. It's a conversation that can get lost in the cancer whirlwind, but it's so important.
Life After Treatment: Survivorship and Follow-Up Care
Treatment ending is a huge milestone, but it's not the end of the journey. The transition into survivorship comes with its own set of challenges – physical, emotional, and practical.
Physically, you may deal with long-term side effects. These can vary but for colorectal cancer patients, issues like altered bowel habits (sometimes called "low anterior resection syndrome" or LARS after rectal surgery), fatigue, neuropathy from chemo, or sexual dysfunction are not uncommon. For women, the latter can be particularly challenging, affecting intimacy and relationships. It's important to address these with your healthcare team, as there are often ways to manage them.
Follow-up care is strict for the first few years, typically involving regular blood tests (checking CEA tumor markers), CT scans, and colonoscopies. This is to catch any recurrence as early as possible. It's a time of "scanxiety" – the anxiety before each follow-up test. That's completely normal.
Emotionally, many survivors experience fear of recurrence, anxiety, depression, or even PTSD. Seeking support from a therapist, counselor, or a dedicated cancer survivorship program is a sign of strength, not weakness. Organizations like the American Cancer Society offer fantastic resources and can help you find local support groups.
Prevention: What Can You Actually Do?
While not all cases are preventable, a huge percentage are linked to modifiable lifestyle factors. This is empowering news.
- Eat for Your Gut: Focus on a diet rich in fruits, vegetables, and whole grains (fiber!). Limit red meat and avoid processed meats like bacon, sausage, and deli meats. It's not about perfection, but consistent patterns.
- Move Your Body: Regular physical activity isn't just for weight management. It reduces inflammation and helps keep your digestive system moving. Aim for 150 minutes of moderate activity per week.
- Maintain a Healthy Weight: Excess body fat, especially around the waist, produces hormones and inflammatory substances that can promote cancer growth.
- Don't Smoke. Limit Alcohol. Smoking is a risk factor for almost every cancer. For alcohol, the recommendation is no more than one drink per day for women.
- And the Number One Thing: GET SCREENED ON TIME. This is non-negotiable. It is the most effective colorectal cancer prevention strategy that exists.
Look, I know health advice can feel overwhelming. You don't have to overhaul your life overnight. Start with one thing. Maybe it's adding more veggies to one meal a day. Maybe it's taking a walk after dinner. Maybe it's finally calling to schedule that screening you've been putting off. That last one is the most important call you can make.
Understanding colorectal cancer in women is about arming yourself with knowledge. It's about knowing your body well enough to recognize when something is off and feeling empowered to speak up. It's about taking proactive steps, like screening, even when you feel fine. The landscape of this disease is changing, with more young women being affected. But our awareness and our actions can change the outcome. Don't wait for the warning signs to become obvious. Be your own best advocate.
POST A COMMENT