Skin Cancer in Women: Signs, Prevention, and What to Know Now
Quick Navigation
- Why Skin Cancer in Women is a Unique Concern
- The Main Types and Their Telltale Signs
- What's Driving the Risk? It's More Than Sunburns
- Prevention: Your Daily Defense Strategy
- The Self-Exam: Your Most Powerful Tool
- What Happens at the Doctor? Diagnosis and Treatment Paths
- The Emotional Side: Fear, Scars, and Moving Forward
- Your Questions, Answered
Let's talk about something that often gets brushed aside until it's a real problem. Skin cancer. For women, the conversation can feel different, loaded with questions about cosmetics, tanning, and spots that just don't look right. I remember a friend who almost didn't get a weird mole on her shoulder checked because it was "just a beauty mark." Turns out, it was early-stage melanoma. That wake-up call made me dive deep into understanding why skin cancer in women deserves its own spotlight.
It's not just a "sun worship" issue. The patterns, the risks, even the way it shows up can have nuances tied to being a woman. Hormones, lifestyle choices, even the types of skincare we use might play a role. It's complex, and frankly, a bit scary. But knowledge is the absolute best defense. So, let's break it down, without the medical jargon, and look at what every woman should know.
Why Skin Cancer in Women is a Unique Concern
You might think skin cancer is skin cancer, right? Well, not exactly. While men statistically have higher rates overall (they're often less diligent with sunscreen, sorry guys), the picture for women has its own distinct features. Melanoma, for instance, is one of the most common cancers in young women (ages 20-39). That's a sobering fact.
Where it shows up differs too. Men tend to get more melanomas on their backs and torsos. Women? They're more common on the legs. But don't let that limit your checks—it can appear anywhere, even in places the sun never touches.
Then there's the hormonal factor. This is a murky area of research, but some studies suggest a possible link between hormonal changes (like during pregnancy or with certain hormone therapies) and the development or worsening of melanoma. The evidence isn't conclusive, but it's enough for doctors to advise close monitoring if you're pregnant and have a history of atypical moles. It adds another layer to the conversation about skin cancer in women that goes beyond just UV exposure.
The Main Types and Their Telltale Signs
Knowing your enemy is half the battle. Skin cancer isn't one single thing. The three main culprits behave differently.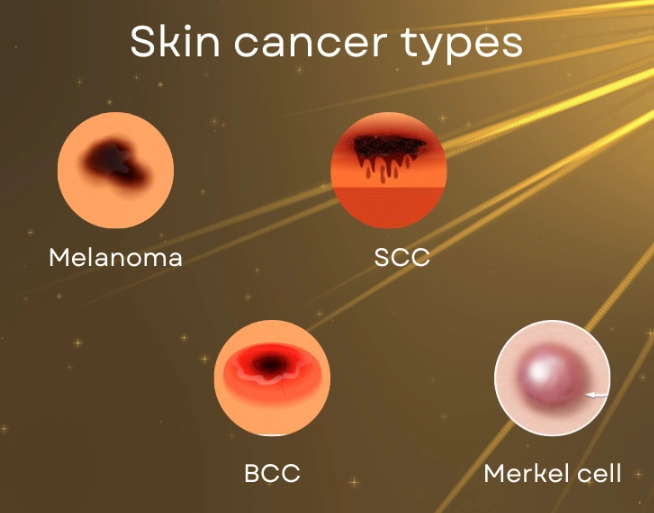
Melanoma: The Aggressive One
This is the one that gets the most attention, and for good reason. It can spread quickly if not caught. But here's the hopeful part: it's also usually visible on the skin early on. The trick is recognizing it. Forget complicated rules for a second. Look for a spot that's changing. That's the biggest red flag.
- The "Ugly Duckling": Does one mole look completely different from all the others on your body? That's a sign.
- Itching or Bleeding: A mole that starts to itch, hurt, or bleed without being irritated needs a professional eye.
- The ABCDEs: Okay, here's the classic guide. It's useful, but don't rely on it alone. Asymmetry (one half doesn't match the other), Border (irregular, scalloped), Color (varied shades of brown, black, red, white, blue), Diameter (larger than a pencil eraser, though they can be smaller), and Evolving (changing in size, shape, or color). The American Academy of Dermatology has excellent visual examples of these ABCDE warning signs.
I find the "E for Evolving" the most critical. A changing spot is a problem spot.
Basal Cell Carcinoma (BCC): The Most Common
This one rarely spreads but it can be locally destructive if left to grow. It often looks like a pearly or waxy bump, or a flat, flesh-colored or brown scar-like lesion. Sometimes it appears as a pinkish patch of skin. It might bleed, scab over, heal, and then repeat the cycle. People often mistake it for a sore that won't heal.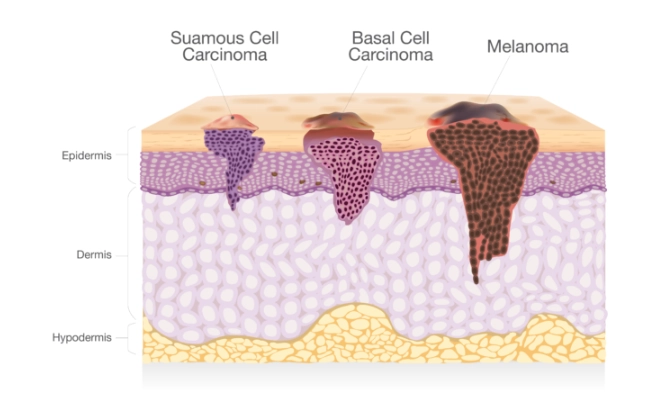
Squamous Cell Carcinoma (SCC): The Scaly Threat
This one tends to be more aggressive than BCC. It often looks like a firm, red nodule or a flat lesion with a scaly, crusted surface. It can also look like a rough patch on the lip or inside the mouth. It's more likely to grow into deeper layers and spread than BCC.
What's Driving the Risk? It's More Than Sunburns
We all know the sun is a major player. But the risk factors for skin cancer in women form a more complete picture when you look at them together.
| Risk Factor | Why It Matters for Women | What You Can Do |
|---|---|---|
| UV Exposure (Sun & Tanning Beds) | Tanning bed use before age 35 increases melanoma risk by 75%. Intermittent, intense sun exposure (think weekend beach trips) is a key risk for melanoma. | Ditch the tanning beds. Period. Seek shade, wear protective clothing, and use broad-spectrum sunscreen daily. |
| Family & Personal History | Having a first-degree relative with melanoma doubles your risk. A personal history of any skin cancer means you're at higher risk for another. | Know your family history. If it's strong, consider annual professional skin exams. |
| Mole Count & Type | Having many moles (especially >50) or atypical (dysplastic) moles increases risk. | Perform regular self-exams to monitor moles for changes. Map them out or take photos. |
| Weakened Immune System | From organ transplants, medications, or conditions like HIV. The body is less able to fight off cancerous changes. | If immunocompromised, be extra vigilant and work closely with your dermatologist. |
| Skin Tone | Fair skin, light eyes, red or blonde hair, and skin that burns/freckles easily equals higher risk. | Sun protection is non-negotiable, regardless of skin tone, but is paramount here. |
See how it stacks up? It's rarely just one thing. It's the combination. A fair-skinned woman with a family history who used tanning beds in college is at a significantly higher risk profile.
Prevention: Your Daily Defense Strategy
Preventing skin cancer in women isn't about living in a cave. It's about smart, consistent habits. Honestly, the skincare industry makes this confusing with a million products. Let's simplify.
Sun Protection That Actually Works
- Sunscreen: Broad-spectrum (UVA/UVB), SPF 30 or higher. Use a shot glass amount for your body and a nickel-sized dollop for your face/neck. Reapply every two hours, or immediately after swimming/sweating. The American Academy of Dermatology's sunscreen guidelines are my go-to resource for cutting through marketing hype.
- Clothing: UPF (Ultraviolet Protection Factor) clothing is fantastic for long days outdoors. A wide-brimmed hat is better than a baseball cap.
- Timing: Seek shade during peak sun intensity (10 a.m. to 4 p.m.).
And let's talk about makeup with SPF. It's a nice bonus, but it's almost never applied thickly enough to provide the stated protection. Don't rely on it as your sole defense. Use a dedicated sunscreen underneath.
The Tanning Bed Talk
This one needs a direct, no-nonsense approach. The World Health Organization classifies tanning beds as a Group 1 carcinogen—the same category as tobacco and asbestos. There is no such thing as a "safe" or "base" tan from a bed. The damage it does to the DNA in your skin cells is cumulative and irreversible. Choosing to use one is choosing to significantly increase your risk of melanoma. It's that stark.

The Self-Exam: Your Most Powerful Tool
You see your skin every day. A dermatologist sees it once a year. You are your own first line of defense. Doing a thorough self-exam once a month takes 10 minutes. Here's how, step-by-step.
- Get Set Up: Use a full-length mirror and a hand-held mirror. Ensure the room is well-lit.
- Start Front & Back: Face the big mirror. Check your face, ears, neck, chest, and belly. Lift your breasts to check the skin underneath. Then turn, check the back of your neck, shoulders, upper back, and the back of your arms.
- Check Sides: With arms raised, look at your left and right sides.
- Arms & Hands: Look at the front and back of your forearms and upper arms. Don't forget your underarms, palms, fingernails, and between fingers.
- Legs & Feet: Sit down. Check the front and sides of your thighs, shins, ankles, and tops of feet. Look between toes, under toenails, and at the soles of your feet. Use the hand mirror for the backs of your thighs and calves.
- The Hard-to-See Spots: This is crucial. Use the hand mirror to check your scalp (part your hair section by section), your buttocks, and your genital area.
Take photos of any moles you're watching. Comparing a photo from month to month is way more accurate than memory.
What Happens at the Doctor? Diagnosis and Treatment Paths
So you found something. Now what? The process is usually straightforward, but the unknown is scary.
First, the dermatologist will look at the spot, often with a dermatoscope—a special magnifying tool. If they're concerned, they'll recommend a biopsy. This is a minor procedure where they numb the area and remove all or part of the spot to send to a lab. It's quick, and stitches are often not needed for small samples.
The biopsy report tells the story: what type of skin cancer it is, how deep it is (for melanoma, this is the Breslow thickness, a critical number), and other features. This information determines the treatment.
Treatment Options: It's Not One-Size-Fits-All
- Excisional Surgery: The standard. The cancer and a margin of healthy skin around it are cut out. For most BCCs and SCCs, this is curative.
- Mohs Surgery: A precise, layer-by-layer removal used for cancers in cosmetically sensitive areas (like the face) or for certain aggressive types. It offers the highest cure rate while sparing healthy tissue.
- Other Options: For superficial cancers, treatments like cryotherapy (freezing), topical creams, or light therapy (photodynamic therapy) might be used.
- For Advanced Melanoma: The landscape has changed dramatically. If melanoma has spread, treatments are no longer just chemotherapy. Immunotherapy (drugs that help your own immune system fight cancer) and targeted therapy (drugs that attack specific genetic mutations in the cancer) have revolutionized outcomes. The American Cancer Society's overview of melanoma treatment details these modern approaches.

The takeaway? Treatment is highly effective when the cancer is caught early. The procedures are outpatient, and recovery is usually quick.
The Emotional Side: Fear, Scars, and Moving Forward
We don't talk about this enough. A skin cancer diagnosis, even a "minor" one, can be emotionally jarring. It's a confrontation with your own mortality. And for women, there's often an added layer of anxiety about scarring, especially if it's on the face.
Let's be real. Yes, there might be a scar. But skilled dermatologic surgeons are artists at minimizing scarring. And a small, faded scar is infinitely better than an untreated cancer. I've spoken to women who said the tiny scar on their nose is now a badge of honor, a reminder to be vigilant.
The fear of recurrence is also real. After treatment, every new spot can trigger anxiety. This is where establishing a good relationship with your dermatologist is key. They become your partner in surveillance, giving you peace of mind.
Your Questions, Answered
Let's tackle some of the specific questions that keep women up at night.
Can I get skin cancer from a mole I've had since birth?
Yes. Congenital moles, especially large ones, have a slightly increased risk of developing into melanoma over a person's lifetime. It's not a guarantee, but it's a reason to keep an eye on them for any changes.
Does my birth control or HRT increase my risk?
The research is ongoing and not totally clear. Some older studies suggested a very slight increase in risk with long-term use of certain oral contraceptives or HRT, but more recent, large studies have not found a consistent link. The general medical consensus is that the benefits of these therapies outweigh any potential, unproven small increase in skin cancer risk. However, if you have a strong family history or other major risk factors, it's a good topic to discuss with both your dermatologist and gynecologist.
I'm pregnant and have a changing mole. What should I do?
See a dermatologist, full stop. Pregnancy can cause benign hormonal changes in moles (darkening, growing), but a changing mole should never be dismissed as "just pregnancy." A biopsy can be safely performed during pregnancy if needed. Delaying could be dangerous.
What's the deal with "clean" sunscreens vs. chemical ones?
This is a huge marketing arena. "Mineral" sunscreens (zinc oxide, titanium dioxide) sit on top of the skin and physically block rays. "Chemical" sunscreens absorb into the skin and absorb UV rays. Both are FDA-approved and effective when used correctly. The best sunscreen is the one you will use generously and reapply. If you have sensitive skin, mineral formulas might be less irritating. The Environmental Working Group's sunscreen guide can be a resource, but remember, their ratings heavily favor minerals. The key is consistent use of any broad-spectrum SPF 30+ product.
How often should I really see a dermatologist?
If you have no personal or family history and no suspicious spots, a baseline exam in your 20s is smart, followed by exams as needed or every few years. If you have significant risk factors (fair skin, many moles, family history, past skin cancer), an annual full-body exam is the standard recommendation. Listen to your doctor's advice based on your personal profile.
Navigating skin cancer in women is about blending awareness with action. It's understanding that your skin tells a story, and you need to learn its language. It's committing to simple, daily protection. It's giving yourself a monthly once-over without panic, just observation. And it's knowing that if something seems off, getting it checked is an act of strength, not worry.
The goal isn't to make you paranoid about every freckle. It's to empower you with the facts so you can enjoy the sun, live your life, and rest easy knowing you're doing what you can to protect the skin you're in. Because when it comes to your health, you're the best advocate you've got.
POST A COMMENT