Fibromyalgia in Women: Symptoms, Diagnosis & Management
If you're a woman dealing with persistent, widespread pain that doctors can't easily pin down, you're not imagining things. You're also not alone. Fibromyalgia predominantly affects women, with estimates from the Centers for Disease Control and Prevention (CDC) suggesting women are about twice as likely as men to be diagnosed. It's more than just "aches and pains"—it's a complex symphony of fatigue, brain fog, and sensory overload that can turn daily life into an exhausting puzzle. For years, I've listened to women describe the frustration of being told "it's all in your head" before finally getting a diagnosis. Let's cut through the noise and talk about what fibromyalgia in women really looks like, why it's different, and most importantly, what you can actually do about it.
What You’ll Find in This Guide
What is Fibromyalgia and Why Does It Affect Women More?
Fibromyalgia isn't joint inflammation or muscle damage you can see on an X-ray. The prevailing theory is that it's a central sensitivity syndrome. Think of your nervous system's volume knob for pain and sensory input being stuck on high. A gentle touch can register as pain. Normal fatigue feels like hitting a wall.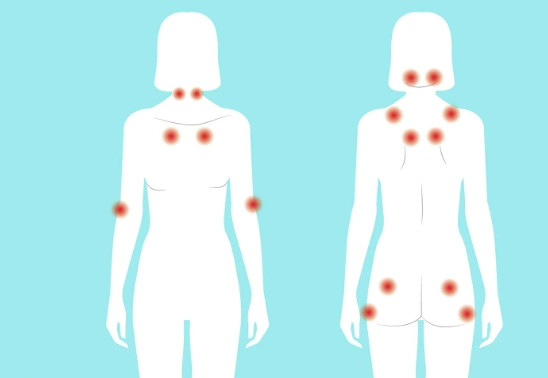
So why women? The disparity isn't fully understood, but it's likely a perfect storm of factors.
Hormones play a undeniable role. Estrogen and progesterone fluctuations across the menstrual cycle, during pregnancy, and in perimenopause can dramatically influence pain perception and symptom severity. Many women report their worst flares in the days leading up to their period. I've had clients track their cycles alongside symptoms for months, and the correlation is often too strong to ignore.
Genetic and immune system differences might make women's nervous systems more prone to this kind of sensitization. There's also the sociological component—women are more likely to seek care for chronic pain, which influences diagnosis rates, but they're also more likely to be dismissed initially.
The Fibromyalgia Symptoms Checklist: Beyond Just Pain
If you only look for pain, you'll miss half the picture. Fibromyalgia is a full-body experience. Here’s a breakdown of what women commonly report.
| Core Symptom | What It Feels Like | Impact on Daily Life |
|---|---|---|
| Widespread Pain | A deep, constant ache, often described as burning, throbbing, or stabbing. It migrates. | Difficulty finding comfortable positions for sleep or work. Hugs can hurt. |
| Crushing Fatigue | Not just tiredness. It's an unrefreshing, bone-deep exhaustion that sleep doesn't fix. | Needing to nap after a shower. The "spoon theory" becomes a lived reality. |
| "Fibro Fog" | Cognitive dysfunction: short-term memory lapses, trouble concentrating, word-finding difficulty. | Forgetting why you walked into a room. Struggling to follow conversations in noisy places. |
| Sleep Disturbances | Difficulty falling/staying asleep, or waking up feeling like you never slept (non-restorative sleep). | Perpetual jet-lagged feeling. Worsens pain and fatigue in a vicious cycle. |
| Sensory Sensitivities | Overwhelm from bright lights, loud noises, strong smells, or certain textures. | Avoiding crowded stores. Needing sunglasses indoors. Clothing tags feel like sandpaper. |
Then there are the frequent companions: irritable bowel syndrome (IBS), headaches, temporomandibular joint (TMJ) disorders, restless legs syndrome, and interstitial cystitis. It's rarely just one thing.
One subtle error I see? Women blaming themselves for the fatigue. "I'm just lazy." No. This fatigue is a core symptom of the condition, a neurological signal, not a character flaw.
How is Fibromyalgia Diagnosed in Women?
There's no single blood test or scan. Diagnosis is clinical, based on history and a physical exam. The old "tender point" exam (pressing 18 specific points) is less emphasized now. The American College of Rheumatology's current criteria focus on:
- Widespread Pain Index (WPI): Pain in at least 4 of 5 body regions.
- Symptom Severity (SS) Scale: Rating the severity of fatigue, unrefreshing sleep, and cognitive symptoms.
- Symptoms lasting at least 3 months with no other underlying condition that explains them.
The diagnostic journey is often long. A 2022 report in the journal Arthritis Care & Research highlighted that delays and misdiagnosis are common. Many women are first treated for depression, anxiety, or told it's just stress.
The goal of testing (blood work, sometimes imaging) is to rule out other conditions like lupus, rheumatoid arthritis, hypothyroidism, or vitamin deficiencies. It's a process of elimination.
Practical Management Strategies That Actually Work
Management is not about finding a magic pill. It's about building a personalized toolkit. The most effective plan is multi-pronged. The National Center for Complementary and Integrative Health (NCCIH) emphasizes a combination of approaches.
1. Movement, But Mindfully
"Exercise more" is terrible advice if you try to do what you used to. The key is graded, low-impact movement. Start with 5 minutes of gentle walking or aquatic therapy. The goal is to gently stimulate your system without triggering a flare. Consistency with tiny amounts beats a 30-minute crash session. Yoga and tai chi are excellent for combining movement with breath awareness.
2. Sleep Hygiene is Non-Negotiable
You can't manage pain without addressing sleep. This isn't just about going to bed early. It's a ritual:
- Cool, dark, quiet room.
- No screens for 60-90 minutes before bed (the blue light disrupts melatonin).
- A consistent wake-up time, even on weekends.
- If pain wakes you, have a calm, non-screen activity ready (gentle stretching, listening to an audiobook). Fighting the wake-up often makes it worse.
3. The Power of Pacing and Planning
This is the single most useful skill. Pacing means breaking activities into smaller chunks with rest before you're exhausted. Clean for 15 minutes, rest for 10. Go to the grocery store on a Tuesday morning, not a Saturday afternoon. It feels counterintuitive—you have a "good day" and want to get everything done. Resist. That overexertion is what often leads to a 3-day crash. Plan your energy like a budget.
4. Medical and Therapeutic Support
Medications like certain antidepressants (e.g., duloxetine, milnacipran) or anti-seizure drugs (e.g., pregabalin) can help modulate the nervous system's pain signals. They are tools, not cures.
Cognitive Behavioral Therapy (CBT) is gold-standard for chronic pain. It's not about thinking your pain away; it's about changing your relationship to it, managing stress (a huge flare trigger), and breaking the fear-avoidance cycle (where you avoid activity for fear of pain, leading to deconditioning and more pain).
The biggest mistake? Jumping from one treatment to the next every two weeks. These interventions—medication, therapy, gentle exercise—often take 6-8 weeks to show noticeable effects. Give them a real chance.
Your Fibromyalgia Questions Answered

Living with fibromyalgia is a marathon, not a sprint. It requires patience, self-advocacy, and a willingness to experiment. Listen to your body—it's giving you information, not betraying you. Connect with supportive communities, whether online or locally. And remember, a diagnosis isn't an end point; it's the starting line for building a life that works for you, on your terms.
POST A COMMENT