Navigating Menopause: A Practical Guide to Effective Symptom Treatment
Let's get straight to it. Menopause isn't a disease to cure; it's a transition to manage. And managing it well means tackling the symptoms that steal your sleep, disrupt your mood, and make you feel like you're hosting a surprise internal sauna several times a day. If you're searching for menopause symptom treatment, you're probably past the point of vague reassurance. You want actionable strategies that work.
I've spent over a decade guiding women through this, and the biggest mistake I see? Treating all symptoms with a single, generic approach. A hot flash, a sleepless night, and a wave of anxiety are different beasts. Effective treatment starts with mapping your specific symptoms to the right tools.
Your Quick Guide to Menopause Relief
Hormone Therapy: The Gold Standard (When It Fits)
Hormone Replacement Therapy (HRT) remains the most effective treatment for moderate to severe vasomotor symptoms (hot flashes, night sweats). It works because it addresses the root cause: declining estrogen.
The conversation around HRT has been a rollercoaster, swinging from panacea to pariah and now, thankfully, to a more nuanced middle ground. Organizations like the North American Menopause Society (NAMS) have clear guidelines: for healthy women under 60 or within 10 years of menopause onset, the benefits of treating disruptive symptoms often outweigh the risks.
Expert Angle: The biggest misconception? That HRT is one thing. It's not. The devil is in the details—the type of estrogen, the dose, and the delivery method (patch, pill, gel, spray). A transdermal patch (through the skin) bypasses the liver, which can be a better choice for women with concerns about blood clots. This is the kind of detail a good menopause specialist will discuss with you.
Who's a good candidate? Generally, women with severe symptoms that impair quality of life, who are in their 40s or 50s, and have no personal history of breast cancer, blood clots, stroke, or heart disease. The decision is intensely personal and must be made with a knowledgeable healthcare provider.
The Non-Hormone Route: Beyond Just Black Cohosh
Not everyone wants or can take hormones. The good news is, the non-hormonal toolkit has expanded.
Prescription Options: Don't overlook these. Medications like low-dose paroxetine (Brisdelle), a selective serotonin reuptake inhibitor (SSRI), are FDA-approved specifically for hot flashes. Gabapentin and clonidine are other non-hormonal prescriptions that can be very effective, especially for night sweats.
Supplements & Herbs: This is where you need a sharp eye. The market is flooded with products making big claims.
- Black Cohosh: The most researched herb. Look for brands that use a standardized extract (like Remifemin®) and have clinical trials behind them. It doesn't work for everyone, but for some, it's a game-changer for hot flashes and mood.
- Phytoestrogens (Soy, Red Clover): The data is mixed. Some women swear by adding high-quality soy (tofu, tempeh, edamame) to their diet. Supplements are trickier—their potency varies wildly.
- Vitamin E & Omega-3s: More foundational support. A small dose of vitamin E (like 400 IU) may slightly reduce hot flash severity. Omega-3s from fish oil support heart and brain health, which is crucial during this transition.
My rule of thumb: Treat supplements like weak medications. Tell your doctor what you're taking. More isn't better, and "natural" doesn't automatically mean safe.
The Lifestyle Layer: Your Daily Foundation
This isn't fluffy advice. Lifestyle changes are the bedrock of symptom management. They make other treatments work better and can be enough on their own for mild symptoms.
Nutrition: It's About What You Add AND Subtract
Cutting back on triggers is half the battle. Spicy food, caffeine, and alcohol are classic hot flash provocateurs. But the other half is adding the right stuff.
Focus on protein at every meal to stabilize blood sugar and mood. Load up on colorful vegetables and fruits for antioxidants and fiber. Calcium and Vitamin D become non-negotiable for bone health—think leafy greens, fortified foods, and maybe a supplement, as recommended by the National Institute on Aging.
Movement: The Unbeatable Mood & Metabolism Regulator
You don't need to train for a marathon. Consistency beats intensity. Aim for a mix:
- Strength Training (2-3x/week): This is critical for fighting muscle loss and supporting bone density. Start with bodyweight squats, lunges, or light dumbbells.
- Cardio (3-5x/week): Brisk walking, swimming, or cycling for 30 minutes helps manage weight, improves sleep, and is a proven mood booster.
- Flexibility & Balance (Daily): Yoga or tai chi are phenomenal. They reduce stress, improve sleep, and enhance balance, which becomes more important as we age.
Sleep & Stress: The Vicious Cycle Breakers
Poor sleep worsens hot flashes and mood swings, which then worsen sleep. You have to break the cycle.
Create a cool, dark, device-free cave for sleep. If you wake up drenched, have a dry nightgown and towel by the bed—sounds simple, but it prevents the frustration of a full bedding change at 3 AM. For stress, find your anchor: 10 minutes of deep breathing, a daily gratitude list, or listening to a calming podcast. It's not extra; it's essential maintenance.
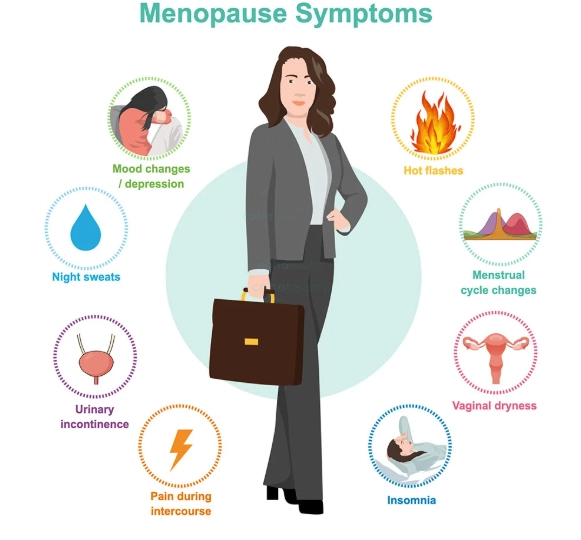
Targeting Specific Symptoms: A Practical Cheat Sheet
Let's get tactical. Here’s a breakdown of common symptoms and the most effective treatment avenues for each.
| Symptom | First-Line Strategies | When to Consider Medical Help |
|---|---|---|
| Hot Flashes / Night Sweats | Layer clothing, cool bedroom, paced breathing, identify & avoid triggers (spicy food, alcohol, stress). | If they occur frequently (10+ per day), disrupt sleep nightly, or persist for months despite lifestyle changes. |
| Mood Swings & Anxiety | Regular cardio exercise, mindfulness/meditation, consistent sleep schedule, limiting caffeine. | If feelings of sadness or anxiety are persistent, interfere with work/relationships, or include loss of interest in activities. |
| Sleep Problems | Strict sleep hygiene (cool, dark, quiet room), no screens before bed, managing night sweats. | If you consistently cannot fall or stay asleep 3+ nights a week for over a month, leading to daytime fatigue. |
| Vaginal Dryness / Pain | Regular use of water-based lubricants, vaginal moisturizers (e.g., Replens), maintaining sexual activity. | If over-the-counter products don't provide enough relief, causing pain during sex or persistent discomfort. |
For vaginal dryness, many women don't realize that low-dose vaginal estrogen (a cream, ring, or tablet) is a local treatment with minimal systemic absorption. It's highly effective and, for most women, carries a very different risk profile than systemic HRT. This is a classic example of a specific solution for a specific problem.
Your Next Steps: Building a Personal Action Plan
Information overload is real. Here’s how to move from reading to doing.
1. Track Your Symptoms for Two Weeks. Use a simple notebook or an app. Note the time, severity, and potential triggers of hot flashes, your sleep quality, and your mood. Patterns will emerge. This data is gold for your doctor.
2. Schedule the Right Kind of Doctor's Appointment. Book a consultation specifically to discuss menopause management. Come with your symptom tracker and a list of questions. If your current doctor dismisses your concerns or isn't knowledgeable, seek out a NAMS-certified menopause practitioner.
3. Implement One Change at a Time. Don't try to overhaul your diet, start intense exercise, and meditate for an hour all on Monday. It won't last. Pick your most bothersome symptom and try one new strategy for it for two weeks. Did adding a daily walk help your mood? Great, keep it. Did cutting evening wine reduce night sweats? Excellent. Build slowly.
Menopause symptom treatment isn't about finding a magic pill. It's about building a personalized toolkit—a combination of medical support, lifestyle habits, and practical tricks—that lets you navigate this transition with your health and sanity intact.
Questions You Might Be Hesitant to Ask
What is the most effective treatment for severe hot flashes during menopause?
Are there natural remedies for menopause that actually work for mood swings?
How long should I expect menopause symptoms to last, and when do treatments stop working?
Can lifestyle changes alone manage menopause symptoms, or is medication always needed?
POST A COMMENT