How to Cure PCOS Permanently: A Realistic Guide to Long-Term Management
Let's be brutally honest from the start. If you're searching for "how to cure PCOS permanently," you're probably exhausted. Exhausted by unpredictable periods, stubborn weight, frustrating acne, and that shadow of worry about fertility. You want a definitive solution, a magic bullet. I get it. I've worked with hundreds of women navigating this, and the first thing we need to clear up is the word "cure."
In strict medical terms, Polycystic Ovary Syndrome is considered a chronic condition. There's no pill you take for two weeks that makes it vanish forever. But here's the crucial, hopeful flip side: it is entirely possible to put PCOS into lasting remission. You can reach a point where your symptoms disappear, your hormones rebalance, your cycles regulate, and you feel like you've gotten your life back. For all practical purposes, that feels like a cure. The path there isn't about quick fixes; it's about systematically addressing the root cause for the long haul.
What You’ll Discover in This Guide
The Uncomfortable Truth About a "PCOS Cure"
Chasing a permanent cure can set you up for disappointment if you don't reframe the goal. The internet is full of "I cured my PCOS in 30 days!" stories. Be skeptical. Often, these are people who made a great change, saw initial improvement, and declared victory. PCOS has a sneaky way of creeping back if you revert to old habits.
Think of it like being an athlete with a tendency for a weak knee. You can't "cure" the predisposition. But you can strengthen the muscles around it, improve your movement patterns, and manage inflammation so effectively that you never experience pain or instability again. You manage it so well it's a non-issue. That's the realistic, powerful goal for PCOS: effective, lifelong management that leads to symptom-free living.
Key Insight: The majority of PCOS cases (some estimates, like those discussed in research from the National Institutes of Health, suggest up to 70-80%) are driven by underlying insulin resistance. This isn't just a side effect; it's often the primary engine driving hormonal chaos—high androgens, irregular ovulation, the works. Address this, and you address the core of the problem for most women.
The Central Problem: It’s All About Insulin Resistance
If you remember one thing from this article, let it be this: for most with PCOS, insulin is public enemy number one.
Here's what happens in simple terms. Your cells stop listening to insulin's signal to take in glucose from your blood. Your pancreas panics and pumps out more insulin. This high insulin level wreaks havoc:
- It tells your ovaries to produce more testosterone (hello, acne and hair growth).
- It tells your liver to produce less Sex Hormone Binding Globulin (SHBG), meaning more of that testosterone is "free" and active.
- It promotes fat storage, particularly around the abdomen.
- It disrupts the signals that trigger ovulation.
See the pattern? It's not that your ovaries are randomly malfunctioning. They're often reacting perfectly logically to the wrong signal—chronically high insulin.
This is why just taking birth control pills or spironolactone often feels incomplete. They manage the symptoms (and can be very helpful tools), but they don't touch the insulin problem. It's like putting a bandage on a leaky pipe without turning off the water.
Your Action Plan for Lasting Remission
Permanent management means building a lifestyle that keeps insulin low and stable. This isn't a temporary diet. It's your new normal. Here’s how to structure it.
1. The Food Foundation: It’s About Carbohydrate Management, Not Just Calories
Forget just eating less. You need to eat smarter for your insulin. A common mistake is switching to "healthy" but still high-carb foods like oatmeal, fruit smoothies, and whole-grain bread all day long. For insulin-resistant PCOS, that's often too much.
The Priority Shift:
- Protein First: Aim for 30+ grams per meal. Chicken, fish, eggs, tofu, Greek yogurt. Protein is incredibly satiating and has a minimal insulin impact.
- Fiber-Rich Veggies: Fill half your plate with non-starchy vegetables (broccoli, leafy greens, peppers, zucchini). The fiber slows glucose absorption.
- Smart Carbs Last: Choose carbs that come with fiber—berries over bananas, quinoa over rice, sweet potato in moderation. A rough starting point for many is aiming for under 100 grams of net carbs (total carbs minus fiber) per day. You may need to go lower temporarily.
- Healthy Fats are Friends: Avocado, olive oil, nuts, seeds. They add flavor, keep you full, and have zero impact on insulin.
This isn't a no-carb diet. It's a controlled-carb, high-satiety approach that gives your insulin system a break.
2. The Exercise Non-Negotiable: Build Muscle
Cardio is fine for heart health, but for insulin resistance, strength training is king. Muscle tissue is your body's largest storage site for glucose. The more muscle you have, and the more you use it, the better your insulin sensitivity.
Aim for 2-3 strength sessions per week. This doesn't mean you need a gym. Bodyweight exercises, resistance bands, dumbbells at home—it all works. The goal is progressive overload: gently challenging your muscles over time.
A Warning on Overtraining: More is not better. Excessive, intense exercise (like daily long-distance running or extreme HIIT) can actually increase cortisol, which may worsen insulin resistance and hormone balance for some women with PCOS. Consistency with moderate strength training beats sporadic exhaustion.
3. Sleep and Stress: The Hidden Levers
Poor sleep and chronic stress raise cortisol. High cortisol tells your body to dump glucose into your bloodstream (a "fight or flight" response), which then requires more insulin. It's a vicious cycle.
Prioritize 7-8 hours of quality sleep. Create a wind-down routine. For stress, find what works for you—10 minutes of meditation, walking in nature, journaling. This isn't fluffy self-care; it's metabolic regulation.
Going Beyond Diet and Exercise: Key Leverage Points
Sometimes lifestyle needs a boost. These are the most evidence-backed supports.
Inositol: This is a B-vitamin-like compound that improves how your cells respond to insulin. Specifically, look for a supplement with a 40:1 ratio of Myo-inositol to D-chiro-inositol, which mimics the body's natural balance. Studies, including those referenced by the International Journal of Endocrinology, show it can improve ovulation, reduce testosterone, and aid metabolic markers. Typical dose is 2-4 grams per day. It's a game-changer for many.
Berberine: This plant compound works similarly to the drug metformin in improving insulin sensitivity. Some research suggests it might be just as effective. A common dose is 500mg, 2-3 times daily with meals. (Consult your doctor before starting, especially if on other medications).
Vitamin D and Magnesium: Deficiencies are common in PCOS and worsen insulin resistance. Get your levels checked. Supplementing to reach optimal levels can provide noticeable support.
What Success Looks Like: A Real Case Study
Let's make this concrete. Sarah, 29, came to me with classic PCOS: no period for 8 months, acne, weight gain concentrated on her belly, and constant cravings.
We didn't do anything extreme. We focused on the pillars above.
- Food: She started eating a protein-rich breakfast (eggs or yogurt) instead of toast or cereal. She aimed for protein + veggies at lunch and dinner, saving her carb portion for dinner (like a serving of sweet potato or lentils).
- Exercise: She began two 30-minute full-body strength sessions per week at home.
- Supplements: She started the 40:1 inositol blend and Vitamin D (her levels were low).
- Mindset: We framed it as "nourishing and strengthening" her body, not punishing it.
The timeline?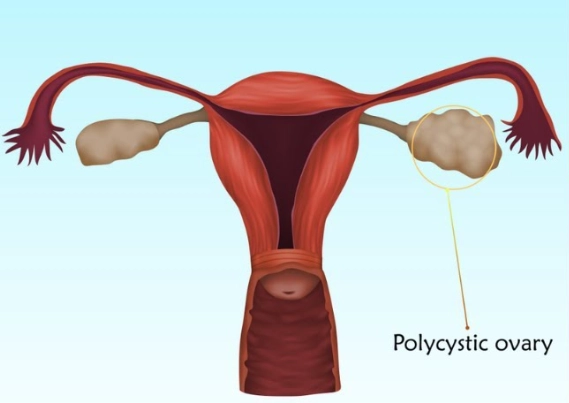
- Week 3: Her energy stabilized, and sugar cravings plummeted.
- Month 2: She got a light period.
- Month 4: Regular 32-day cycle returned. Acne cleared significantly.
- Month 8: She'd lost 18 pounds, but more importantly, her fasting insulin and testosterone blood tests had normalized.
Two years later, she maintains these habits seamlessly. Her PCOS is in remission. She's not "cured"—if she went back to her old diet for months on end, symptoms would likely return. But she has a system that works, and it's sustainable. That's the win.
Your Top PCOS Management Questions Answered
The journey to managing PCOS for good is a shift in identity. It's moving from someone who "has a broken thing to fix" to someone who understands her body's unique metabolism and cares for it accordingly. It's building daily habits that keep insulin in check. There's no expiration date on that. When you do that, you stop chasing a mythical cure and start living in a state of effective, permanent management. That's where true freedom lies.
POST A COMMENT