Understanding Urinary Tract Infections: Symptoms, Treatment & Prevention
Quick Guide
- What Does a UTI Actually Feel Like? Spotting the Symptoms
- Why Me? The Common Causes and Risk Factors
- Getting a Diagnosis: What to Expect at the Doctor's Office
- UTI Treatment: From Antibiotics to Home Comfort
- Prevention: How to Stop UTIs Before They Start
- Complicated UTIs and When to Worry
- Your UTI Questions, Answered (The Real Ones People Ask)
- Final Thoughts: Taking Control of Your Urinary Health
Let's be honest. If you've ever had one, you know. That sudden, urgent need to run to the bathroom, only to be met with a sharp, stinging pain. It's frustrating, it's uncomfortable, and it can really throw your day off. You're not alone. Millions of people deal with urinary tract infections every single year.
I remember a friend calling me once, almost in tears, because she thought something was seriously wrong. She just didn't know what was happening. Turns out, it was a classic case of a UTI. The lack of clear information out there is surprising, honestly. You get a mix of old wives' tales, confusing medical jargon, and ads for cranberry juice.
So, let's cut through the noise. This isn't a dry medical textbook. Think of it as a long chat with someone who's done the research, talked to doctors, and sifted through the good and bad advice. We're going to cover everything—what it really feels like, why it happens, what you should actually do about it, and most importantly, how to stop it from coming back.
What Does a UTI Actually Feel Like? Spotting the Symptoms
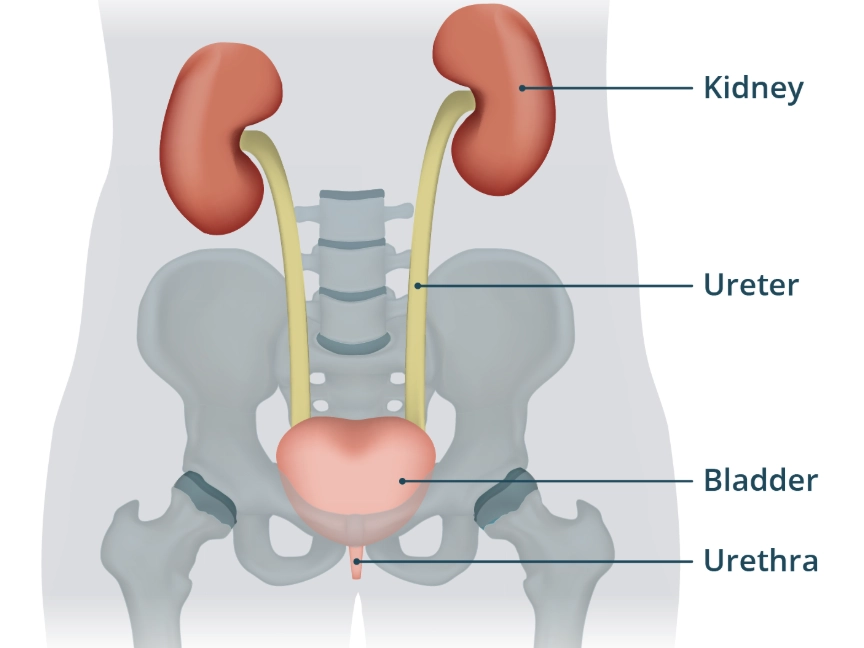
It doesn't always start with a bang. Sometimes it's just a little "off" feeling. But knowing the signs can help you act fast. The symptoms of a urinary tract infection can vary a bit depending on which part of your system is affected, but there's a common theme of irritation and urgency.
Here’s the rundown of what most people experience:
- A burning sensation when you pee. This is the hallmark. It’s not subtle.
- A persistent, urgent need to urinate, even if you just went and only a few drops come out.
- Cloudy, dark, bloody, or strange-smelling urine. Your pee is a great indicator.
- Pelvic pain or pressure, especially in women, often felt in the center of the pelvis and around the pubic bone.
- Passing small amounts of urine frequently. It feels like your bladder is never empty.
Now, if the infection travels up to your kidneys, that's a more serious situation called pyelonephritis. The symptoms get more intense and systemic. We're talking fever, chills, nausea, vomiting, and pain in your upper back and sides (flank pain). That's not a "wait-and-see" scenario—that's a "call your doctor or go to urgent care right now" situation.
 If you have fever and back pain with urinary symptoms, don't wait.
If you have fever and back pain with urinary symptoms, don't wait.Lower UTI vs. Upper UTI: Knowing the Difference
It's helpful to break it down because the level of concern is different. A lower urinary tract infection is annoying and painful. An upper UTI (kidney infection) can make you feel truly ill and requires prompt medical attention.
| Feature | Lower UTI (Cystitis/Urethritis) | Upper UTI (Pyelonephritis - Kidney Infection) |
|---|---|---|
| Primary Location | Bladder and/or urethra | Kidneys |
| Common Symptoms | Burning with urination, urgency, frequency, pelvic pressure, cloudy urine | All lower UTI symptoms PLUS fever (>100.4°F), chills, nausea/vomiting, flank/side/back pain |
| Severity | Generally uncomfortable but not systemic | More severe, systemic illness; can lead to complications if untreated |
| Typical Action | Contact primary doctor for appointment | Contact doctor immediately or seek urgent/emergency care |
Men can get UTIs too, though it's less common. When they do, they might also experience rectal pain. For older adults, sometimes the only sign is new confusion or agitation, which makes it tricky to diagnose.
Why Me? The Common Causes and Risk Factors
Okay, so we know what it is. The next big question is: why did it happen? In the vast majority of cases, a urinary tract infection is caused by bacteria that live in your gut, like E. coli, finding their way into your urinary tract. The design is a bit flawed, to be frank—the exit point is close to where these bacteria hang out.
Let's look at the things that can tip the scales and increase your risk. Some you can control, some you can't, but knowing them is power.
Top Risk Factors for Developing a UTI:
- Female Anatomy: This is the big one. Women have a shorter urethra than men, which means bacteria have a shorter distance to travel to reach the bladder. It's simple geometry, and it's unfair.
- Sexual Activity: Intercourse can introduce bacteria into the urinary tract. Some people call this "honeymoon cystitis." It's very common.
- Certain Types of Birth Control: Diaphragms and spermicidal agents can disrupt the natural bacterial balance and increase risk.
- Menopause: The drop in estrogen causes changes in the urinary tract that make it more vulnerable to infection.
- Urinary Tract Blockages: Kidney stones or an enlarged prostate can trap urine in the bladder, creating a breeding ground for bacteria.
- A Suppressed Immune System: Diabetes and other conditions that impair your immune system make it harder to fight off invaders.
- Recent Urinary Procedure: Using a catheter or having a cystoscopy can introduce bacteria.
I think the sexual activity point causes a lot of unnecessary stress and confusion. It doesn't mean you or your partner are "unclean." It's just a mechanical reality of anatomy. Knowing this helps you take practical steps, like peeing after sex, without feeling shame or blame.
Getting a Diagnosis: What to Expect at the Doctor's Office
You've got the symptoms, you suspect it's a UTI. What next? You'll need a proper diagnosis to get the right treatment. This isn't something you should try to tough out or solely treat with over-the-counter remedies.
When you see a doctor or visit a clinic, they'll start by asking about your symptoms. Be blunt. Tell them about the burning, the urgency, the cloudiness. They've heard it all before. Then, they'll almost certainly ask for a urine sample.
The Urine Test Process
You'll get a little cup and be sent to the bathroom. They usually want a "clean-catch, midstream" sample. This means you start peeing, then catch some of the urine from the middle of the stream in the cup. It helps reduce contamination from skin bacteria.
The sample then goes through two main checks:
- Urinalysis: A quick dipstick test right in the office. It looks for signs of infection like white blood cells (leukocytes), red blood cells, and nitrites (which some bacteria produce). A positive dipstick is a strong indicator.
- Urine Culture: This is the gold standard. The lab tries to grow bacteria from your sample to confirm an infection and, crucially, to identify exactly which bacteria is causing it. This takes 24-48 hours but tells the doctor which antibiotic will work best.
For uncomplicated lower UTIs in young, healthy women, a doctor might diagnose based on symptoms and a urinalysis alone and prescribe an antibiotic right away. For recurrent infections, complicated cases, or suspected kidney infections, a culture is essential.
UTI Treatment: From Antibiotics to Home Comfort
Alright, let's talk about fixing the problem. The cornerstone of treating a bacterial urinary tract infection is, unsurprisingly, antibiotics. They kill the bacteria causing the trouble. But it's not just about taking a pill; it's about doing it right.
Your doctor will choose an antibiotic based on the likely bacteria, your health history, and local resistance patterns. Common first-line choices include trimethoprim/sulfamethoxazole (Bactrim), nitrofurantoin (Macrobid), and fosfomycin (Monurol).
For a simple bladder infection, symptoms often improve within 1-2 days of starting antibiotics. A kidney infection might require a longer course or even intravenous antibiotics in severe cases.
What About Pain Relief?
Antibiotics tackle the root cause, but they don't instantly erase the pain. That burning sensation can linger for a day or two. Here's what can help while the antibiotics do their job:
- Phenazopyridine (Pyridium, Azo): This is an over-the-counter urinary analgesic. It doesn't treat the infection—it just numbs your urinary tract lining to relieve burning and urgency. It turns your urine bright orange or red, which is startling but harmless. Don't use it for more than two days without consulting a doctor, as it can mask symptoms if the infection isn't improving.
- Heating Pad: A simple, drug-free way to ease pelvic and abdominal discomfort.
- Stay Hydrated: This seems counterintuitive when peeing hurts, but diluting your urine can make it less acidic and less irritating as it passes. Water is your best friend.
I'm skeptical of the dozens of "UTI cure" teas and supplements you see online. Some might offer supportive symptom relief, but they are not a substitute for antibiotics for a confirmed bacterial infection. Relying on them alone can allow the infection to worsen.
Prevention: How to Stop UTIs Before They Start
This is the holy grail, especially if you're someone who gets them frequently. While you can't eliminate risk entirely, you can definitely stack the odds in your favor. Most of this is about simple, consistent habits.
Let's bust a myth first: Cranberry juice. The evidence is mixed. Some studies suggest compounds in cranberries (proanthocyanidins) might prevent bacteria from sticking to the bladder wall. Others show minimal benefit. If you like it and it doesn't bother you, it's probably not harmful (choose low-sugar options), but don't rely on it as your sole shield. Cranberry supplements are a more concentrated option, but talk to your doctor before starting.
Proven Prevention Strategies (The Real Stuff):
- Drink Plenty of Fluids, Especially Water: This flushes bacteria out of your system regularly. Aim for clear or pale yellow urine.
- Don't Hold It In: Go to the bathroom when you feel the urge. Stagnant urine is a better breeding ground.
- Wipe From Front to Back: Always. This prevents spreading bacteria from the anal region to the urethra.
- Pee Shortly After Sexual Intercourse: This helps flush out any bacteria that may have been introduced.
- Reconsider Your Birth Control: If you get frequent UTIs and use a diaphragm or spermicide, chat with your gynecologist about alternatives.
- Avoid Potentially Irritating Products: Douches, powders, and strong soaps in the genital area can disrupt the natural microbiome and cause irritation.
- For Postmenopausal Women: Talk to your doctor about topical vaginal estrogen therapy. It can help restore the health of vaginal and urinary tissues, significantly reducing UTI risk.
It sounds simple, but consistency is key. Making these habits automatic is your best long-term defense against recurrent urinary tract infections.
Complicated UTIs and When to Worry
Not all UTIs are straightforward. Doctors categorize them as "uncomplicated" or "complicated." An uncomplicated UTI is in a healthy, non-pregnant person with a normal urinary tract. Everything we've mainly discussed so far falls into that category.
A complicated urinary tract infection happens when there are other factors that increase the risk of treatment failure or serious illness. This includes:
- UTIs in men (due to anatomical differences and potential prostate involvement).
- Pregnant women.
- People with diabetes, a weakened immune system, or kidney disease.
- Infections caused by antibiotic-resistant bacteria.
- Structural abnormalities in the urinary tract (like stones, strictures, or catheters).
Treatment for complicated UTIs often requires longer antibiotic courses (sometimes 7-14 days instead of 3-5), different antibiotic choices based on culture results, and closer follow-up. It might also involve seeing a specialist, like a urologist, to address any underlying anatomical issues.
- Fever over 101°F (38.3°C) with urinary symptoms.
- Shaking chills or severe nausea/vomiting.
- Severe pain in your side, back, or abdomen.
- Confusion or sudden mental changes (especially in the elderly).
- If your symptoms don't start improving after 2-3 days on antibiotics.
Your UTI Questions, Answered (The Real Ones People Ask)
Final Thoughts: Taking Control of Your Urinary Health
Dealing with a urinary tract infection is a pain, literally. But it doesn't have to be a mystery or a source of constant anxiety. The key is knowledge and proactive habits.
Listen to your body. Those early twinges of burning or urgency are signals. Act on them by increasing your water intake and contacting your healthcare provider. Don't fall into the trap of thinking you have to suffer through it or that it's "just something you have to live with." Modern medicine has straightforward solutions.
Focus on the prevention habits that work: hydration, timely bathroom breaks, and post-sex hygiene. They're boring, but they're effective. And if you're in the recurrent infection camp, have that deeper conversation with a doctor. There are more advanced management plans available.
Your health is worth the effort. A clear understanding of urinary tract infections—from that first suspicious symptom to long-term prevention—puts you back in the driver's seat. No more dread, just practical knowledge and a plan.
POST A COMMENT