Lung Cancer in Women: Risks, Symptoms, and Survival Guide
Quick Guide
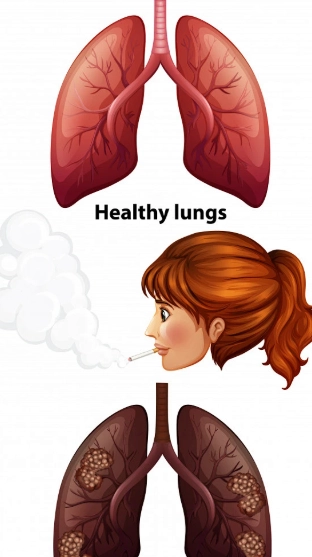
Let's talk about something serious. Lung cancer. For years, the conversation was dominated by images of older men who smoked. But the picture has changed, dramatically. More and more, we're seeing lung cancer in women, and the story isn't always the same. It can be different in how it shows up, what causes it, and even how it behaves. I've read the stats, and honestly, some of them are startling. Did you know it's the leading cause of cancer death among women in the United States, even ahead of breast cancer? That fact alone should make us all sit up and pay closer attention.
Maybe you're here because you have a cough that won't quit. Maybe you're worried about a family member. Or perhaps you're a non-smoker who thinks this doesn't apply to you. I used to think that way too. But the reality of lung cancer in women is complex, and understanding it could be life-saving. This isn't meant to scare you—it's meant to arm you with knowledge. We're going to walk through everything from the silent risks you might not know about, to the symptoms that are easy to brush off, all the way to what happens after a diagnosis.
Why Are Women Getting Lung Cancer? The Risk Factors Beyond Cigarettes
Okay, let's get the big one out of the way first. Yes, smoking is still the number one risk factor for lung cancer in women. But here's the thing. The rise in cases isn't just about smoking. In fact, a significant portion of women diagnosed with lung cancer have never smoked, or smoked very little. So what's going on?
It turns out the risk landscape for women is unique. There are factors at play that might not affect men in the same way.
Key Takeaway: While smoking is a major driver, assuming it's the only cause means missing a huge part of the story for women. The biology is different.
Top Risk Factors for Lung Cancer in Women
- Smoking and Secondhand Smoke: This is the big one. Current and former smokers are at high risk. But don't underestimate secondhand smoke. Living with a smoker or working in a smoky environment for years counts as a serious exposure. The American Cancer Society has clear data on how this increases risk.
- Radon Gas: This is the second leading cause of lung cancer overall, and it's a silent, invisible threat. Radon is a radioactive gas that comes from the natural breakdown of uranium in soil and rock. It can seep into homes through cracks in the foundation. The scary part? You can't see or smell it. The U.S. Environmental Protection Agency (EPA) recommends testing your home—it's cheap and easy.
- Family History and Genetics: If a first-degree relative (parent, sibling, child) had lung cancer, your risk goes up. This is true even if you don't smoke. Researchers are still untangling the specific genetic links, but the family connection is real.
- Other Environmental Exposures: This includes things like asbestos (think older buildings, certain industries), arsenic in drinking water, and some forms of air pollution. Occupational exposures can be a factor, though regulations have made this less common than in the past.
- Hormonal Factors: This is where it gets interesting and specific to women. Some studies have suggested a possible link between estrogen and the development or progression of certain lung cancers. Women who take hormone replacement therapy (HRT) or who started menstruating earlier or entered menopause later might have a slightly different risk profile. The research isn't totally conclusive yet, but it's a active area of study. The National Cancer Institute (NCI) follows this research closely.
I find the radon thing particularly unnerving. It's completely random based on where you live. Testing your home is one of the most practical, proactive things you can do, and so few people actually do it.
Spotting the Signs: Symptoms of Lung Cancer in Women
This is the part where listening to your body is everything. The symptoms of lung cancer can be incredibly sneaky. They often mimic other, less serious conditions like a cold, bronchitis, or just being run down. Women sometimes report slightly different symptoms than men, too, like more frequent coughing or shortness of breath early on.
The problem is, by the time symptoms are obvious, the cancer may have already advanced. That's why knowing the early, subtle signs is crucial.
Heads Up: If any of these symptoms persist for more than a few weeks without a clear explanation (like a known infection), it's time to see a doctor. Don't fall into the trap of thinking "it's probably nothing."
Here’s a checklist of symptoms to be aware of:
- A Cough That Won't Go Away: This is the most common one. A new cough that lingers, or a "smoker's cough" that gets worse or changes in sound.
- Coughing Up Blood: Even a small amount of rust-colored phlegm or blood. This is a major red flag.
- Chest Pain: Pain that's worse with deep breathing, coughing, or laughing. It's often constant and dull.
- Hoarseness: A change in your voice that lasts.
- Shortness of Breath: Getting winded doing tasks that never used to be a problem.
- Unexplained Weight Loss and Loss of Appetite: Losing weight without trying is a classic sign of many cancers.
- Feeling Tired or Weak All the Time: Fatigue that doesn't get better with rest.
- Infections That Keep Coming Back: Like bronchitis or pneumonia that seems to recur in the same part of the lung.
- Less Common Signs (Sometimes Seen More in Women): Shoulder or arm pain (if a tumor presses on a nerve), swelling in the face or neck, or even clubbing of the fingernails (where the nails curve down and the fingertips enlarge).
See what I mean? Half of these could be explained away so easily. That persistent cough? Allergies. The tiredness? Just busy. This is what makes lung cancer in women so dangerous—its masterful disguise.
Getting a Diagnosis: The Tests and Scans
So you or your doctor are concerned. What happens next? The diagnostic process can feel overwhelming, but it's a step-by-step journey to get answers.
It usually starts with imaging. A simple chest X-ray might spot a mass, but a CT scan is the real workhorse for getting a detailed look. If something suspicious is found, the next step is to get a sample of tissue—a biopsy—to confirm if it's cancer and, if so, what type.
| Test Type | What It Does | What to Expect |
|---|---|---|
| Chest X-ray | First look for masses or abnormalities in the lungs. | Quick, painless. Often the initial screening tool. |
| CT Scan (Computed Tomography) | Provides a detailed, 3D image of the lungs. Can find much smaller nodules than an X-ray. | You lie on a table that slides into a ring-shaped scanner. It's painless but you need to hold still. |
| PET Scan (Positron Emission Tomography) | Used after a nodule is found. Shows if it's metabolically active (like cancer) and if cancer has spread. | A small amount of radioactive sugar is injected. Cancer cells absorb it and "light up" on the scan. |
| Biopsy (Various Types) | Removes a small piece of tissue for lab analysis. This is the only way to confirm cancer. | Can be done via a needle through the chest wall (CT-guided), through a bronchoscope (tube down the throat), or surgically. |
| Molecular/Genetic Testing | Done on the biopsy sample. Looks for specific gene mutations (like EGFR, ALK, ROS1) that drive the cancer's growth. | This is critical! It determines if you are eligible for targeted therapies, which can be game-changers, especially for non-smoking women with lung cancer who often have these mutations. |
The waiting period for these results is arguably the hardest part. But that molecular testing? It's non-negotiable in my opinion. It moves treatment from a one-size-fits-all approach to a personalized plan. Don't let your doctor skip this step.
Treatment Options: It's Not Just Chemo Anymore
The world of lung cancer treatment has exploded with new options in the last decade. This is good news. The old days of just chemotherapy and radiation are over. Now, treatment is highly tailored to the type of lung cancer, its stage, and your specific genetic profile.
The main types of lung cancer are Non-Small Cell Lung Cancer (NSCLC), which is about 85% of cases, and Small Cell Lung Cancer (SCLC), which is more aggressive and strongly linked to smoking. Most lung cancer in women is NSCLC.
The Modern Treatment Toolkit
- Surgery: The goal is to remove the tumor and nearby lymph nodes. This is often the best chance for a cure if the cancer is caught early and hasn't spread. Types range from removing a small wedge of lung to an entire lobe (lobectomy).
- Radiation Therapy: Uses high-energy beams to kill cancer cells. It can be used before surgery to shrink a tumor, after surgery to kill remaining cells, or as the main treatment if surgery isn't possible. Techniques like stereotactic body radiotherapy (SBRT) are precise and powerful for small tumors.
- Chemotherapy: Uses drugs to kill fast-growing cells throughout the body. It's often used before or after surgery, or for more advanced cancers. The side effects are tough, but management has improved.
- Targeted Therapy: This is a huge breakthrough. If your cancer has a specific genetic mutation (like EGFR, ALK, ROS1, BRAF), you can take a pill that specifically targets and blocks that mutation. These drugs often work better and have fewer side effects than chemo for people whose cancers have these markers. They are frequently effective for non-smoking women with lung cancer.
- Immunotherapy: Another revolution. These drugs don't attack the cancer directly. Instead, they take the "brakes" off your own immune system, allowing it to recognize and attack cancer cells. Drugs like pembrolizumab (Keytruda) have changed survival rates for many.
"The shift to targeted therapies and immunotherapy has been the most significant advance in my career. For the right patients, it transforms a terminal diagnosis into a manageable chronic condition." – This sentiment is echoed by many oncologists specializing in thoracic cancers.
Treatment is rarely just one thing. It's often a combination, like chemo plus immunotherapy, or surgery followed by targeted therapy. Your medical team will build a plan for you.
Life After Diagnosis: Survival, Support, and Mindset
Let's talk numbers, but let's keep them in perspective. The overall 5-year survival rate for all stages of lung cancer is improving, but it's still lower than for many other cancers because it's often found late. However, if caught at a localized stage (before it spreads), the 5-year survival rate jumps dramatically—to over 60%.
That's why early detection is the holy grail. For women at high risk (like long-term smokers), low-dose CT screening is recommended. The U.S. Preventive Services Task Force has guidelines on who should get screened. If you qualify, it's a scan that could save your life.
Survival is more than a statistic. It's about quality of life. Managing symptoms like fatigue and breathlessness, dealing with the emotional rollercoaster, and finding your "new normal" are all part of the journey. Support groups—specifically for women with lung cancer—can be invaluable. Organizations like the American Lung Association offer resources and connections.
The stigma is real too. The assumption that "you must have smoked" adds an unnecessary layer of guilt and shame. It's a terrible burden to carry on top of a serious illness. This is a disease, full stop. Compassion, not judgment, is what's needed.
Look, navigating a potential or actual diagnosis of lung cancer in women is tough. The information is dense, the emotions are high, and the system can be confusing. My goal here was to pull it all together in one place—the risks you might not have considered, the symptoms you shouldn't ignore, and the modern hope that exists in treatment.
It's a lot to take in. Bookmark this page. Share it with a friend. The more we understand about the unique face of lung cancer in women, the better we can fight it, support each other, and push for more research and early detection methods that work for everyone.
POST A COMMENT