Understanding Your Menstrual Cycle Symptoms: A Comprehensive Guide
For years, I just gritted my teeth through the cramps and blamed myself for the week of irritability before my period. It was just something to endure, a messy inconvenience. Then I started tracking—not just the start date, but the subtle shifts. The energy surge around day 12. The specific craving for dark chocolate and red meat a week out. The tight lower back that always showed up 48 hours before the main event. It wasn't random chaos; it was a predictable, albeit sometimes frustrating, pattern. Understanding menstrual cycle symptoms isn't about pathologizing a normal process. It's about decoding the signals your body sends throughout the month, so you can work with your rhythm, not against it.
This guide walks you through the four distinct phases, the common (and less common) symptoms tied to each, and—most importantly—actionable strategies to manage them. Forget one-size-fits-all advice. What helps during your period is different from what helps the week before.
What's in This Guide
The Four-Phase Breakdown: Symptoms Stage by Stage
Your cycle is more than just "period" and "not period." Hormones like estrogen and progesterone rise and fall in a specific sequence, creating four phases with unique physiological landscapes. Here’s what you might feel in each.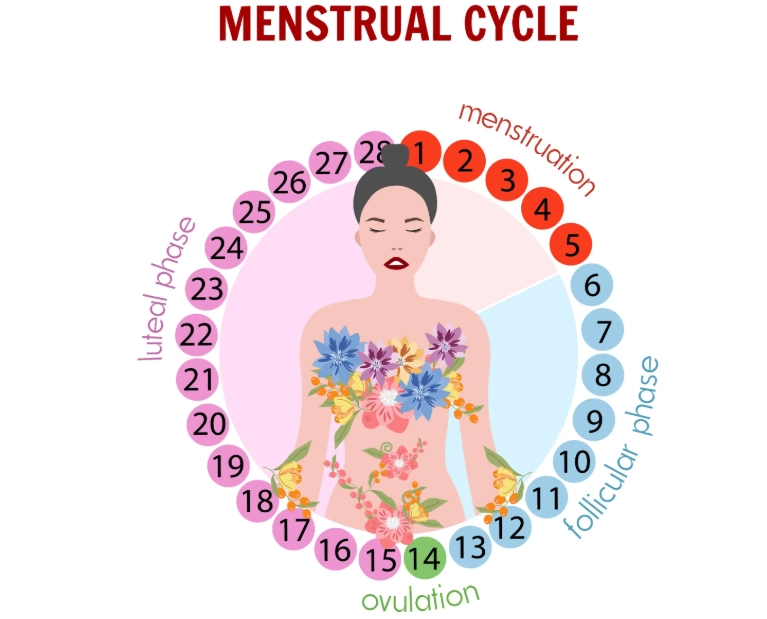
1. Menstrual Phase (Days 1-5ish): The Reset
This is when the uterine lining sheds. Hormone levels are at their lowest point.
What you might feel:
- Cramping (Dysmenorrhea): That aching, squeezing sensation in your lower abdomen, sometimes radiating to your back or thighs. It's caused by prostaglandins, hormone-like chemicals that make the uterus contract.
- Fatigue and low energy. Your body is doing work.
- Bloating (though often relief from pre-period bloat begins here).
- Headaches triggered by the hormonal drop.
- Loose stools or diarrhea (prostaglandins affect the bowels too).
- A sense of inward focus or desire for rest. This isn't a flaw; it's a biological cue.
2. Follicular Phase (Days 1-13ish): The Ascent
This phase overlaps with menstruation and continues until ovulation. Estrogen begins its steady climb, rebuilding the uterine lining.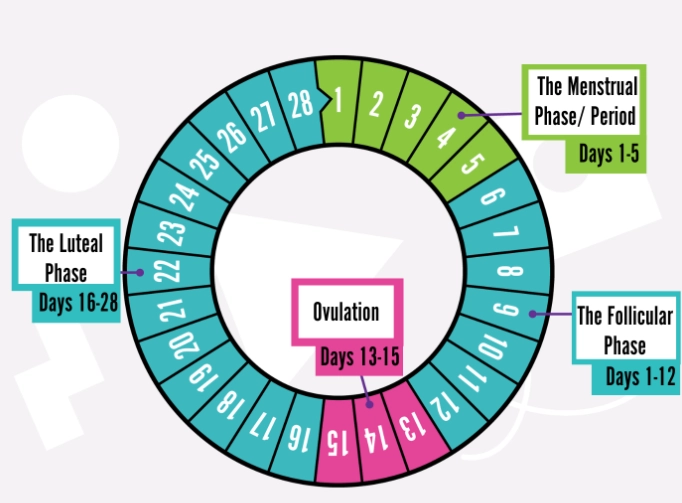
What you might feel:
- Increasing energy and motivation. This is often when you feel most socially engaged and ready to tackle new projects.
- Improved mood and mental clarity. Rising estrogen can boost serotonin.
- Light, less noticeable cervical fluid that may be sticky or creamy.
- By the end of this phase, you might feel a surge of creativity and optimism.
Many people feel their best during the late follicular phase. It's a great time for intense workouts, important meetings, or social planning.
3. Ovulation (Day 14ish): The Peak
A surge of Luteinizing Hormone (LH) triggers the release of an egg. Estrogen peaks just before this.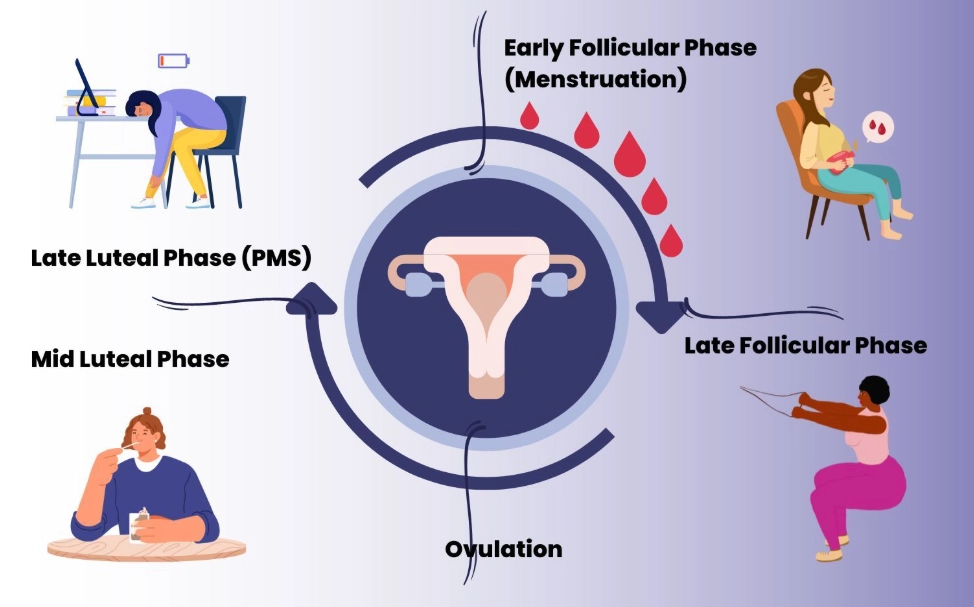
What you might feel:
- Mittelschmerz: A brief, one-sided pinching or aching sensation when the ovary releases the egg. It can last minutes or hours.
- Vaginal discharge becomes clear, slippery, and stretchy—like raw egg whites.
- Increased libido. Nature's not-so-subtle nudge.
- A subtle rise in basal body temperature after ovulation occurs.
- Some feel confident, charismatic, and more physically vibrant.
- Light spotting or breast tenderness for some.
4. Luteal Phase (Days 15-28ish): The Waiting Game
After ovulation, the corpus luteum forms and secretes progesterone, which stabilizes the uterine lining. If pregnancy doesn't occur, this structure disintegrates, leading to the hormone drop that starts your period.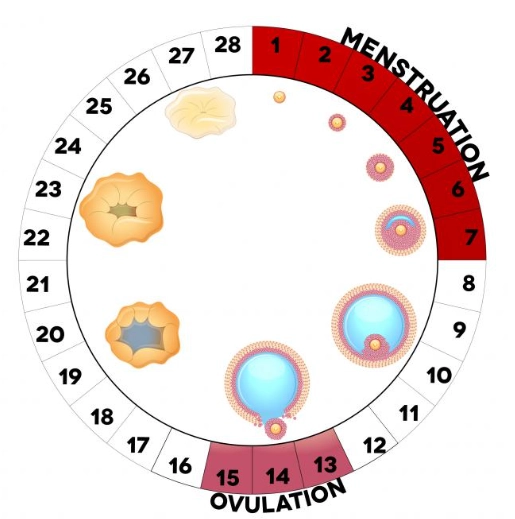
What you might feel (Hello, PMS):
- Mood changes: Irritability, anxiety, sadness, or mood swings. Progesterone can have a depressive effect for some.
- Physical symptoms: Breast tenderness and swelling, bloating, acne flare-ups.
- Appetite changes: Intense cravings for carbs, chocolate, or salty foods.
- Fatigue and sleep disturbances.
- Headaches.
- Constipation (progesterone slows down digestion).
- A gradual decline in energy toward the end of the phase.
PMS symptoms typically appear in the last 5-7 days of the luteal phase. The severity varies wildly from person to person.
Beyond the Calendar: Smart Symptom Tracking Strategies
Marking "Day 1" on a calendar is a start, but it doesn't tell the full story. Tracking symptoms does two crucial things: it predicts your personal pattern and provides concrete data if you need to seek medical help.
I used a simple notes app at first. Now I see the value in dedicated apps or a paper journal. The key is consistency. Jot down a few things each evening.
Track These Core Items:
- Physical: Energy level (1-10), any pain (location, severity), digestion, breast tenderness, skin state, sleep quality.
- Emotional/Mental: Mood descriptor (irritable, calm, joyful, anxious), focus, motivation, libido.
- Cycle-Specific: Bleeding (light/medium/heavy), cervical fluid consistency, any spotting.
After two or three cycles, patterns emerge. You'll see if your low mood reliably hits on day 22, or if your cramps are worst on day 2. This knowledge is power. You can plan a light workday for your predicted low-energy day or schedule that important dinner out for your high-energy follicular phase.
If your symptoms are severe, this log becomes invaluable for your doctor. Saying "I have bad PMS" is vague. Showing them: "For 7 days pre-period, my anxiety peaks at an 8/10, I have debilitating fatigue, and I get migraines" is specific and actionable. Organizations like the American College of Obstetricians and Gynecologists (ACOG) note that symptom diaries are a key diagnostic tool for conditions like PMDD (Premenstrual Dysphoric Disorder).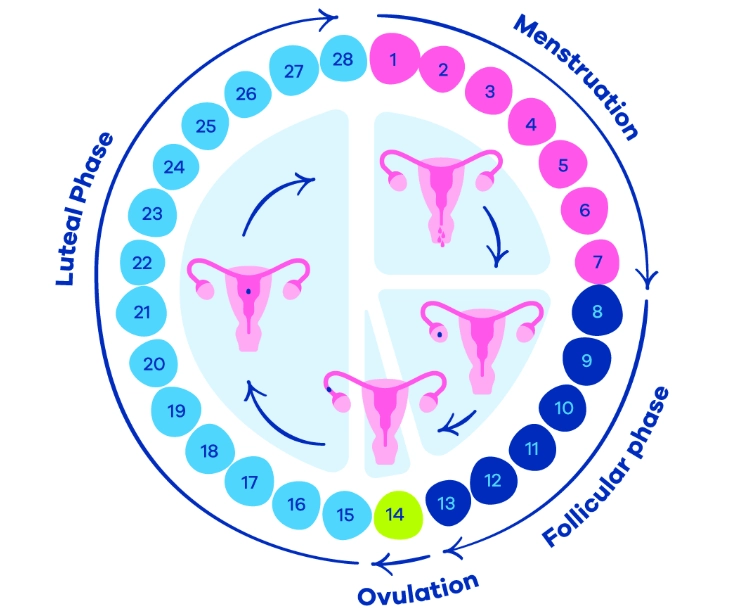
Phase-Specific Management Tactics That Actually Work
Generic advice like "reduce stress" or "exercise" isn't wrong, but it's not precise. Your body's needs change. Here’s a phase-by-phase approach.
Menstrual Phase: Prioritize Rest and Relief
Fighting the fatigue here is a losing battle. Lean into it.
- For cramps: Heat is a proven muscle relaxant. A heating pad on your lower abdomen for 20 minutes can be as effective as a pill for some. Start NSAIDs (ibuprofen, naproxen) at the first sign of cramps to block prostaglandins.
- Movement: Swap high-intensity workouts for gentle yoga, walking, or stretching. It increases blood flow without depleting you.
- Nutrition: Focus on iron-rich foods (leafy greens, lentils, red meat if you eat it) to replenish what's lost. Stay hydrated to combat bloating from dehydration.
Follicular & Ovulation Phases: Capitalize on Energy
This is your productivity and social window.
- Schedule demanding tasks, creative projects, and intense workouts (like HIIT or strength training). Your body is primed for it.
- Your pain tolerance is higher. This is a good time for dentist appointments or other potentially uncomfortable tasks.
- Socialize, network, pitch ideas. Your rising confidence is a real asset.
Luteal Phase: Support and Stabilize
The goal here is to mitigate the PMS crash. Proactive beats reactive.
- Nutrition Tweaks:
- Complex carbs: Your body is craving them for serotonin. Choose oats, sweet potatoes, and whole grains over candy to avoid sugar crashes.
- Magnesium: This mineral can ease cramps, improve sleep, and stabilize mood. Think spinach, almonds, dark chocolate (80%), pumpkin seeds.
- Reduce salt & processed foods: To help with water retention and bloating.
- Movement: Steady-state cardio (brisk walking, cycling, swimming) can boost mood and reduce bloating better than exhaustive exercise, which might increase cortisol and worsen symptoms.
- Stress Management: This is non-negotiable. The luteal phase makes you more vulnerable to stress. Prioritize evening wind-down routines, say no to extra obligations, and practice breathing exercises. A 10-minute meditation can blunt the edge of irritability.
- Sleep Hygiene: Progesterone makes you sleepy but can disrupt sleep quality. Keep your room cool and dark, and avoid screens before bed.
| Symptom | Quick-Action Relief Tips | Long-Term Support Strategy |
|---|---|---|
| Menstrual Cramps | Heating pad, start NSAIDs early, gentle cat-cow stretches. | Regular exercise, consider supplementing Magnesium Glycinate. |
| PMS Bloating | Drink plenty of water, avoid carbonated drinks, peppermint tea. | Reduce processed foods & salt intake in luteal phase; increase potassium (bananas, avocados). |
| Premenstrual Mood Swings | 5-minute box breathing, take a walk outside, call a supportive friend. | Consistent sleep schedule, complex carbs at meals, discuss options with doctor if severe. |
| Mid-Cycle Ovulation Pain | Heat, rest, gentle movement like walking. | Track to confirm pattern; if severe, discuss with gynecologist. |
A common mistake I see? People try to push the same rigid routine all month. It's exhausting. Sync your life to your cycle, not the other way around. Plan your big presentation for your follicular phase. Schedule a cozy movie night for when you know you'll be in your luteal phase. It's a form of self-respect.
Your Top Menstrual Symptom Questions, Answered
The journey with your cycle is lifelong. Symptoms can change after pregnancy, with age, or due to stress. The goal isn't to eliminate all symptoms—that's unrealistic. It's to understand their language, respond with kindness and practical support, and recognize when a symptom is shouting for medical attention. Start by tracking one cycle. Just one. You might be surprised by the story it tells.
POST A COMMENT