What Causes Low Iron in Women: 10 Key Reasons & How to Fix It
Your Reading Map: Key Sections Ahead
Let's talk about something that hits close to home for so many women I know, maybe for you too. That dragging fatigue that coffee just can't fix. The brain fog that makes you forget why you walked into a room. The pale skin, the brittle nails, the constant feeling of being cold. If you're nodding along, there's a good chance iron deficiency is playing a role. It's incredibly common, yet so many of us just push through, blaming stress or a busy life. But understanding what causes low iron in women is the first step to feeling like yourself again.
I remember a friend of mine, let's call her Sarah. She was a powerhouse—full-time job, two kids, always on the go. But for months, she was just wiped. She chalked it up to being a mom. Turns out, her iron levels were in the tank. Her story isn't unique. In fact, according to the World Health Organization, iron deficiency is the most common nutritional disorder globally, and women are disproportionately affected. So, why is that? Why are we so prone to it?
This isn't just about eating more spinach (though that can help). The reasons behind low iron in women are woven into our biology, our lifestyles, and sometimes, underlying health conditions we might not even be aware of. We're going to dig into all of it—the obvious culprits and the sneaky ones you might not have considered.
The Core Reasons: What Causes Low Iron in Women?
When we ask "what causes low iron in women," the answer is rarely one single thing. It's usually a combination of factors stacking up. Your body needs iron to make hemoglobin, the protein in red blood cells that carries oxygen. If you don't have enough, your tissues and organs don't get the oxygen they need. That's when the fatigue and other symptoms kick in. For women, several key areas create the perfect storm for deficiency.
Dietary Factors: You Might Not Be Getting What You Think
This is the first place most people look, and for good reason. But it's more nuanced than just "not eating enough iron."
Not Enough Heme Iron: Iron from animal sources (heme iron)—like red meat, poultry, and fish—is absorbed much more easily by your body than iron from plants (non-heme iron). If you follow a vegetarian or vegan diet, you need to be extra strategic. You're consuming iron, but your body might only be absorbing a small fraction of it.
Quick Tip: Pairing plant-based iron sources (like lentils, spinach, or tofu) with vitamin C (like bell peppers, oranges, or strawberries) can boost absorption significantly. A lentil soup with a squeeze of lemon? Perfect.
Poor Absorption, Not Just Intake: You could be eating iron-rich foods but still have low levels. Certain things block iron absorption. Calcium supplements taken with a meal, the tannins in tea and coffee, and the phytates in whole grains and legumes can all act as little locks, preventing your body from taking in the iron. I used to drink a strong black tea with my morning oatmeal—a classic absorption-blocking combo without realizing it.
Restrictive Diets and Fads: Extreme dieting, cutting out entire food groups without proper planning, or following trendy but unbalanced eating plans can quickly lead to shortfalls in iron and other critical nutrients.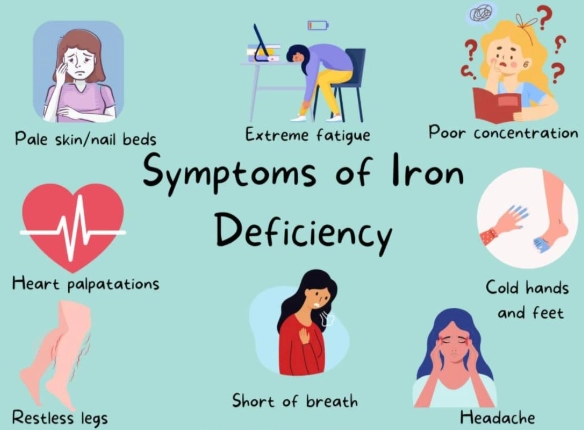
The Big One: Blood Loss
This is arguably the most significant factor specifically for women. Every month, through menstruation, women lose blood—and with it, iron. The heavier your periods, the greater the risk.
Heavy Menstrual Bleeding (Menorrhagia): This is a major driver of what causes low iron in women. Soaking through a pad or tampon every hour for several consecutive hours, passing large clots, or having periods that last longer than 7 days are all signs. Conditions like uterine fibroids, adenomyosis, or simply hormonal imbalances can cause heavy bleeding. Many women think their heavy flow is normal because it's always been that way, but it can be a primary reason for chronic iron depletion.
Other Sources of Blood Loss: It's not just periods. Frequent blood donation, regular use of NSAIDs like ibuprofen or aspirin (which can cause stomach bleeding), or underlying gastrointestinal issues like ulcers, gastritis, or even celiac disease can lead to slow, chronic blood loss that adds up over time. This is often a silent contributor.
A Point of Frustration: Sometimes, women's heavy periods are dismissed by doctors as "just something to deal with." If you feel your symptoms are being minimized, it's okay to seek a second opinion. Persistent fatigue is not normal.
Life Stages That Demand More Iron
Our iron needs aren't static. They skyrocket during certain phases of life, and if intake doesn't keep up, deficiency follows.
Pregnancy and Breastfeeding: During pregnancy, a woman's blood volume increases dramatically to support the growing baby and placenta. The body needs double the amount of iron. It's no wonder that iron deficiency anemia is so common in pregnancy. Postpartum, blood loss during delivery and breastfeeding (which diverts nutrients) can continue the drain. Prenatal vitamins are crucial here for a reason.
Adolescence: The rapid growth spurt during the teen years requires more iron to build new muscle and blood cells. When this is combined with the start of menstruation and sometimes erratic or restrictive eating habits, it creates a high-risk window for deficiency.

Underlying Health Conditions That Interfere
Sometimes, the root of the problem isn't about what's going in or coming out, but what's happening inside that prevents proper use of iron.
Gut Health Issues: Conditions like Celiac disease, inflammatory bowel disease (Crohn's, ulcerative colitis), or even atrophic gastritis (common in older adults) damage the lining of the gut, which is where iron is absorbed. You could be eating plenty, but your damaged gut just can't take it in. This is a critical piece of the puzzle that often gets missed.
Chronic Inflammation: Diseases that cause long-term inflammation, like autoimmune disorders (rheumatoid arthritis, lupus), chronic kidney disease, or even persistent obesity, can alter how your body manages iron. The body sequesters iron away in storage, making it less available for making new red blood cells, a condition sometimes called "anemia of chronic disease."
Let's look at some of these common and not-so-common causes in a simple table. It helps visualize where the problem might be starting.
| Cause Category | Specific Examples | Why It Leads to Low Iron |
|---|---|---|
| Diet & Absorption | Vegetarian/Vegan diet, high tea/coffee intake with meals, calcium supplements with food. | Reduces intake or blocks absorption of non-heme iron in the gut. |
| Blood Loss | Heavy menstrual periods, frequent nosebleeds, stomach ulcers, regular aspirin use. | Directly depletes iron lost through hemoglobin in blood. |
| Increased Demand | Pregnancy, breastfeeding, adolescence growth spurts. | The body's requirement for iron exceeds what is typically consumed. |
| Medical Conditions | Celiac disease, Crohn's disease, gastric bypass surgery, chronic kidney disease. | Damages absorption sites in the gut or disrupts the body's iron regulation system. |
How Do You Know For Sure? Signs and Diagnosis
So, you're wondering if what causes low iron in women might be affecting you. The symptoms can be vague and creep up slowly, making them easy to ignore or attribute to other things.
The Classic Signs:
- Extreme fatigue and weakness: The hallmark symptom. Not just sleepiness, but a deep, unshakable exhaustion.
- Pale skin and "pale" insides: Look at your lower eyelid—it should be a vibrant red, not a light pink or white.
- Shortness of breath and heart palpitations: Your heart and lungs are working overtime to deliver limited oxygen.
- Headaches, dizziness, and lightheadedness.
- Brittle nails, hair loss, and cold hands/feet.
- Strange cravings (Pica): Wanting to chew ice, clay, dirt, or paper is a surprisingly common and specific sign of iron deficiency.
Getting the Right Test: Don't self-diagnose based on symptoms alone. You need a blood test. A simple Complete Blood Count (CBC) is a start, but to truly diagnose iron deficiency, doctors need to look at:
- Ferritin: This is your iron storage protein. Low ferritin is the clearest early sign of depleted iron stores, even before anemia shows up. This is a key test many women need to ask for.
- Serum Iron & TIBC: These measure the iron in your blood and your blood's capacity to carry iron.
- Hemoglobin & Hematocrit: These measure the actual oxygen-carrying capacity of your blood. They are low in iron deficiency anemia.
The Mayo Clinic provides excellent resources on interpreting these tests. A doctor can put the whole picture together. If your ferritin is low, you're iron deficient, full stop, even if your hemoglobin is still in the "normal" range. That's called non-anemic iron deficiency, and it can make you feel just as terrible.
Fixing the Problem: What Actually Works
Okay, so you've identified potential causes and gotten a diagnosis. Now, how do you fix it? The approach depends on the severity and the root cause.
Dietary Changes: Food First
Improving your diet is foundational, but it requires a bit of know-how.
Pro-Tip for Absorption: Have a glass of orange juice with your iron-fortified cereal. Skip the coffee or tea for at least an hour before and after your main iron-containing meal. Take calcium supplements at a different time of day.
Top Iron-Rich Foods to Focus On:
- Heme Iron (Best absorbed): Lean red meat (beef, lamb), organ meats (liver—in moderation), poultry, shellfish (clams, oysters), sardines.
- Non-Heme Iron (Pair with Vitamin C): Lentils, beans, tofu, tempeh, spinach, kale, fortified cereals, pumpkin seeds, quinoa.
Honestly, relying solely on spinach is a myth. You'd have to eat a massive amount to meet your needs because of the absorption issue. Diversify your plate.
Iron Supplements: A Necessary Boost
For many women with significant deficiency, diet alone won't be enough to replenish stores quickly. Supplements are often necessary, but they come with caveats.
Choosing and Taking Them: Doctors often prescribe ferrous sulfate, ferrous gluconate, or ferrous fumarate. The key is elemental iron content. They can cause side effects like constipation, nausea, and stomach upset. Here's what helps:
- Start with a lower dose and work up.
- Take it with a small amount of food (though this slightly reduces absorption, it's better than not taking it at all due to nausea).
- Take it with vitamin C (like a small glass of orange juice).
- Never take it with calcium-rich foods, coffee, or tea.
A Warning: Do not start high-dose iron supplements without a confirmed deficiency. Too much iron is toxic and dangerous. Always work with a healthcare provider. The UK's National Health Service (NHS) has clear guidelines on iron supplement use.
Treating the Underlying Cause
This is the most important part. If you don't address what's causing the loss or poor absorption, you'll just be pouring iron into a leaky bucket.
- For heavy periods, talk to your gynecologist about options like hormonal IUDs, birth control pills, or other medications to reduce flow.
- For suspected gut issues, a referral to a gastroenterologist for testing (like an endoscopy) might be needed.
- Managing chronic inflammatory conditions with appropriate treatment can help improve iron utilization.

Common Questions Women Ask About Low Iron
Putting It All Together: Your Action Plan
Figuring out what causes low iron in women in your specific case is a personal detective story. Here’s a simple roadmap:
- Listen to Your Body: Don't ignore persistent fatigue, paleness, or strange cravings. They are signals.
- Get Tested Properly: Request a full iron panel, including ferritin, from your doctor. Don't settle for just a CBC.
- Review Your Lifestyle: Look at your diet, your menstrual flow, any medications, and your overall health.
- Address the Root Cause: Work with your doctor to manage heavy periods, investigate gut health, or treat underlying conditions. This is the long-term fix.
- Replenish Strategically: Use a combination of diet optimization and, if needed, well-chosen supplements under medical guidance.
- Re-test: After 3-4 months of intervention, get your blood work done again to see if you're improving.
Low iron isn't a life sentence. It's a manageable condition. But the first step is taking your symptoms seriously and understanding the complex web of factors that contribute to it. For more detailed, science-backed information on iron and health, the NIH Office of Dietary Supplements and the Cleveland Clinic are fantastic, trustworthy resources to bookmark.
The bottom line? Your energy and vitality matter. Unraveling what causes low iron in women is a powerful act of self-care. It’s about moving from just getting through the day to truly thriving in it.
POST A COMMENT