How to Test for Lupus in Women: The Complete Diagnostic Guide
Quick Navigation
- First, Understanding the Beast: What is Lupus Anyway?
- The Red Flags: Common Symptoms That Might Prompt Testing
- The Diagnostic Journey: It's a Process, Not an Event
- Breaking Down the Tests: The Blood Work and Beyond
- The Official Rulebook: Diagnostic Criteria (SLICC vs. ACR)
- What to Do and Ask at the Doctor's Appointment
- After the Diagnosis: Next Steps and Management
Let's be real, getting a lupus diagnosis isn't like getting a strep test. There's no single, quick swab that says "yep, that's lupus." It's more of a puzzle, and for women—who make up about 90% of lupus patients—figuring out how to test for lupus in women can feel incredibly overwhelming. You might be dealing with strange symptoms that come and go, seeing different doctors, and getting confusing blood work back. I've talked to so many women in this exact spot, feeling lost in the medical maze.
The process is tricky because lupus, or Systemic Lupus Erythematosus (SLE) if we're using the full name, is a master of disguise. It's an autoimmune disease where your body's defense system gets confused and starts attacking your own tissues. This can affect almost any part of you—skin, joints, kidneys, heart, even your brain. Since it mimics so many other conditions, knowing how to test for lupus in women properly is crucial to avoid years of misdiagnosis and frustration.
Think of this guide as your roadmap. We're going to walk through everything from the first suspicious symptoms to the specific blood tests, the official criteria doctors use, and what to do after you get an answer. My goal is to demystify the process so you can have more informed conversations with your healthcare team.
First, Understanding the Beast: What is Lupus Anyway?
Before we jump into tests, it helps to know what we're looking for. Lupus isn't a bacteria or a virus you can just culture. It's a chronic, systemic autoimmune condition. "Systemic" is the key word here—it means it can be body-wide. Your immune system, which is supposed to fight off invaders like the flu, starts producing antibodies that target your own cells and organs. This leads to inflammation, which is at the root of all those varied symptoms.
Why women? Honestly, the science isn't 100% settled, but hormones like estrogen are strongly suspected to play a major role. That's why symptoms often flare around menstrual cycles, during pregnancy, or with certain hormone therapies. It's a classic example of a disease where sex differences matter a great deal in both how it presents and how it's managed.
The Red Flags: Common Symptoms That Might Prompt Testing
Lupus doesn't announce itself with one clear symptom. It whispers, and then sometimes shouts, with a collection of issues. If you're a woman experiencing a combination of these, it might be time to ask your doctor about lupus. Here's what often shows up on the radar:
- The Fatigue That Isn't Just Tired: This isn't "I need a nap" tired. It's a deep, bone-crushing exhaustion that doesn't improve with rest. It can be debilitating.
- The Butterfly Rash (Malar Rash): A classic sign, but not everyone gets it. It's a red or purplish rash across the cheeks and bridge of the nose, shaped like a butterfly. It often appears or worsens after sun exposure.
- Joint Pain and Swelling: Stiff, aching, swollen joints, especially in the morning. It often affects the hands, wrists, and knees and can mimic arthritis.
- Unexplained Fevers: Low-grade fevers (around 100°F) that come and go without an obvious infection.
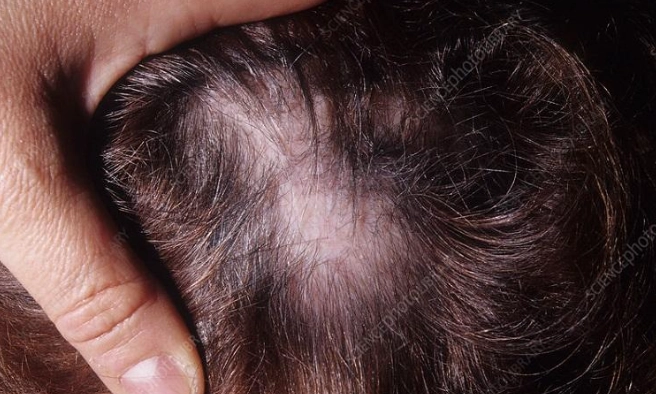
- Hair Loss: Not just thinning, but sometimes patchy hair loss or hair becoming brittle and breaking easily.
- Raynaud's Phenomenon: Fingers and toes that turn white, then blue, then red in response to cold or stress. It's a circulation issue.
- Mouth or Nose Sores: Ulcers inside the nose or mouth, usually painless.
- Chest Pain: Pain when taking a deep breath (pleurisy) from inflammation of the lining around the lungs or heart.
- Kidney Problems: Often silent at first, but signs can include foamy urine (excess protein), high blood pressure, or swelling in the legs. This is a serious complication.
- Neurological Symptoms: Brain fog ("lupus fog"), headaches, memory issues, or even seizures in severe cases.
See what I mean? It's a long, weird list. One day it's your joints, the next it's a rash, and all the while you're just utterly drained. This variability is exactly why understanding how to test for lupus in women requires looking at the whole picture, not just one symptom.
The Diagnostic Journey: It's a Process, Not an Event
So, you've talked to your primary care doctor about your symptoms. What happens next? The path to diagnosis usually involves a partnership between you, your primary doctor, and often a specialist called a rheumatologist. Rheumatologists are the detectives for autoimmune diseases like lupus.
The process isn't linear. It involves a detailed medical history, a thorough physical exam, and a series of laboratory tests. Doctors are essentially gathering clues. They need to rule out other conditions that can look similar, like rheumatoid arthritis, thyroid disease, or chronic fatigue syndrome. This is where patience, unfortunately, becomes a necessary virtue.
Breaking Down the Tests: The Blood Work and Beyond
This is the core of how to test for lupus in women. When you go for testing, your doctor will likely order a panel of blood and urine tests. Let's make sense of what they're looking for.
The Cornerstone: Antinuclear Antibody (ANA) Test
This is almost always the first blood test ordered when lupus is suspected. It checks for antinuclear antibodies—proteins your immune system might be making that attack the nucleus of your own cells. A positive ANA is very common in lupus (over 95% of patients have it), but it's also found in other autoimmune diseases and even in some healthy people.
So, a positive ANA is a clue, not a verdict. The lab will also report a "titer" (like 1:80, 1:320) and a "pattern" (like homogeneous, speckled). Higher titers are more suggestive of an autoimmune process. The pattern can give the rheumatologist additional hints, but it's not diagnostic by itself.
The Lupus-Specific Antibody Tests
If the ANA is positive (or sometimes even if it's negative but suspicion is high), doctors dig deeper with more specific tests. These antibodies are much more closely associated with lupus.
| Test Name | What It Detects | Why It Matters for Lupus |
|---|---|---|
| Anti-dsDNA | Antibodies against double-stranded DNA. | Highly specific for lupus. High levels often correlate with active disease, especially kidney involvement (lupus nephritis). |
| Anti-Smith (Anti-Sm) | Antibodies against Smith proteins. | Also highly specific for lupus, but found in only about 10-30% of patients. Its presence is a strong indicator. |
| Anti-Ro/SSA and Anti-La/SSB | Antibodies against Ro and La proteins. | Common in lupus and Sjögren's syndrome. Associated with sun-sensitive rashes, sicca symptoms (dry eyes/mouth), and neonatal lupus in pregnancy. |
The General Health and Inflammation Markers
These tests paint a picture of how your body is being affected overall.
- Complete Blood Count (CBC): Checks for anemia (low red blood cells), leukopenia (low white blood cells), or thrombocytopenia (low platelets)—all common in lupus.
- Erythrocyte Sedimentation Rate (ESR) & C-Reactive Protein (CRP): Nonspecific markers of inflammation in the body. They can be elevated when lupus is active.
- Complement Levels (C3, C4): Measures proteins that are consumed during immune system activity. Low C3 or C4 levels can indicate active lupus, especially in the kidneys.
- Creatinine and Urinalysis: Crucial for checking kidney function. Lupus nephritis is a serious complication. The urinalysis looks for protein, blood, or cellular casts in the urine, which signal kidney inflammation.

The Official Rulebook: Diagnostic Criteria (SLICC vs. ACR)
Doctors don't just guess. They use standardized criteria to ensure an accurate diagnosis. There are two main sets, and rheumatologists often use a blend of both clinical judgment and these guidelines.
The American College of Rheumatology (ACR) established the first widely used criteria. The more recent SLICC (Systemic Lupus International Collaborating Clinics) classification criteria are also very common. You can find a detailed breakdown of the SLICC criteria on the Lupus Foundation of America website.
In simple terms, these criteria work on a point system. You need to meet a certain number of clinical (symptoms) and immunologic (blood test) criteria. For example, under SLICC, you might need a positive ANA plus at least one clinical criterion (like the butterfly rash or kidney disease) and one immunologic criterion (like a positive Anti-dsDNA). Or, you might need a biopsy-proven kidney lupus (lupus nephritis) with a positive ANA or Anti-dsDNA.
The Takeaway: The process of how to test for lupus in women relies on matching your unique symptom profile with specific lab findings, measured against these established medical criteria. It's about fitting the puzzle pieces together until the picture of lupus becomes clear.
What to Do and Ask at the Doctor's Appointment
Feeling prepared can ease the anxiety. Here’s how to make the most of your visit if you're seeking answers about lupus.
- Keep a Symptom Journal: For a few weeks before your appointment, jot down your symptoms, their severity, what time of day they occur, and anything that makes them better or worse (like sun exposure, stress, or your menstrual cycle). This is gold for your doctor.
- Bring Your History: Know your family history of autoimmune diseases (lupus, rheumatoid arthritis, thyroid disease, etc.).
- Ask Direct Questions:
- "Based on my symptoms, do you think testing for lupus is appropriate?"
- "Which specific blood tests are you ordering, and what does each one tell us?"
- "How long will it take to get these results, and what's the next step once we have them?"
- "At what point would you refer me to a rheumatologist?"
- Get Copies of Your Results: Don't just wait for a phone call. Ask for a copy of your lab reports. This helps you track your own health and be prepared for specialist visits.

After the Diagnosis: Next Steps and Management
So, let's say the puzzle is solved, and a diagnosis is made. This isn't an end point; it's the beginning of a new chapter focused on management. While there's no cure for lupus yet, it is very treatable. The goal is to achieve remission (little to no disease activity) and prevent flares and organ damage.
Treatment is highly individualized but often includes:
- Medications: These can range from anti-inflammatories (NSAIDs) and antimalarials (like hydroxychloroquine, which is a cornerstone for most patients) to corticosteroids and stronger immunosuppressants for more serious organ involvement.
- Lifestyle as Medicine: This is non-negotiable. Strict sun protection (sunscreen, hats), a balanced diet, regular gentle exercise when possible, stress management techniques, and prioritizing sleep become critical parts of your routine.
- Regular Monitoring: You'll have regular check-ups with your rheumatologist, including repeat blood and urine tests to monitor disease activity and medication side effects.
- Building a Support Team: This includes your rheumatologist, primary care doctor, and possibly specialists like a nephrologist (for kidneys) or dermatologist (for skin). Don't underestimate the value of a good therapist or a support group—the emotional toll is real.

The journey of learning how to test for lupus in women ultimately leads here: to a plan. A diagnosis, while challenging, provides a name for what you're fighting and a path forward for treatment. It replaces uncertainty with action.
Figuring out how to test for lupus in women is about connecting the dots between your lived experience and medical science. It requires a proactive approach, a knowledgeable medical team, and a dose of patience. The tests—from the initial ANA to the specific antibody panels and kidney checks—are the tools that bring clarity out of confusion.
If you see yourself in the symptoms described here, take that first step. Talk to your doctor, start that symptom diary, and get the ball rolling. A diagnosis is the key that unlocks access to proper treatment, support, and the chance to manage your health and reclaim your life. For the most current and detailed medical information, always refer to authoritative sources like the Lupus Foundation of America or the Mayo Clinic's lupus overview.
POST A COMMENT